Title: Effectiveness of Aquatic Therapy in Treating Women Diagnosed With Fibromyalgia Compared to Land-based Therapy or Usual Care.
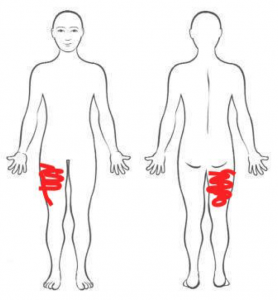
Introduction: Fibromyalgia syndrome (FMS) is characterized by widespread musculoskeletal pain and fatigue. More commonly diagnosed in females than males between ages of 30-50 yrs old. Symptoms include: lack of energy, fatigue, weakness, sleep and cognitive disturbances, stiffness, tender points, IBS, tension type headaches, anxiety and/or depression. According to ACR diagnostic criteria, person must experience symptoms for more than 3 month, and feel tenderness in at least 11 of 18 tender points. There is no cure for FMS, however light exercises with stretching, jogging, swimming, aerobic, have been shown to help with pain and psychological factors by reducing sedentary life styles.
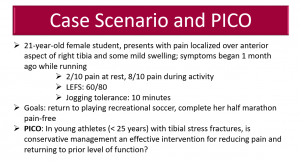
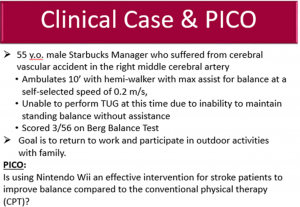
Case Scenario: Patient is a 36 years old female presenting to an outpatient Physical Therapy clinic with complains of joint pain in bilateral knees, shoulders, elbows and lower back pain. She reports fatigue on exertion and low stamina. Patient was diagnosed with fibromyalgia 2.5 years ago. She reports she doesn’t know how exactly her symptoms started but suspects that she never fully recovered after a flu virus 3 years ago. Patient feels stiffness and pain in the morning which gets a little better as the day goes but then gets worse in the evening again. Patient reports her pain goes up to 5-6/10 at worst, 2-3 at best and 3 currently. Taking warm baths and meditating sometimes helps ease the pain a little, but the pain is mostly there all the time. She has good and bad days where pain fluctuates and she noticed that too much physical activity increases her symptoms. Patient is currently unemployed due to the fact that she is unable to perform her work requirements because of the pain and fatigue that she is experiencing every day. Her occupation is a massage therapist which requires moderate physical activity level. Patient reports feeling depressed at times due to her symptoms and is unable to participate in recreational activities. She gets tired very easily with minimal activity which she tries to limit during her bad days. Patient enjoys walking her dog but is unable to walk for more than 2 blocks due to exertional fatigue which makes her very upset. Patient gained 20 pounds over the last 2 years due to limited physical activity. Patient denies any changes in bowel or bladder movement and reports no numbness or tingling in her lower or upper extremities. She is currently taking Lyrica for her symptoms which was prescribed by her Rheumatologist but is still not getting adequate relief with the medicine. No other health issues have been identified. Patient was referred to Physical Therapy for evaluation and treatment to help with her fibromyalgia symptoms. Patient did not have Physical Therapy in the past and believes that it could be beneficial for her. Patient goals for the therapy are to decrease her pain level, increase strength, minimize exertional fatigue so she can walk her dog for more than 2 blocks, and increase her stamina.
During Physical Examination patient displayed weakness in all major upper and lower extremity muscles with grades 3-4/5, bilateral tightness in hamstrings and gastroc-soleus, and minor tightness in bilateral IT band. Lumbar active ROM is limited and painful in all directions. She was tender to the touch around lower back and sacral area and displayed decreased lumbar lordosis. Patient’s back and hip extension was examined in a standing position due to inability to lay prone because of the tenderness in her knees. During examination patient was tender to the touch in bilateral knees, shoulders and elbows. Her shoulders active ROM was within normal limits. Patient presented with slight fatigue during examination and was irritated due to her pain.
Outcomes:
NPRS: Worst 5-6/10, Best 2-3, Now 3
Physical activity: Exertional fatigue/able to walk no more then 2 blocks
MMT: weakness in all major UE/LE muscles with grades 3-4/5
Palpation: Tenderness in bilateral knees, shoulders, elbows, and lower back and sacral area
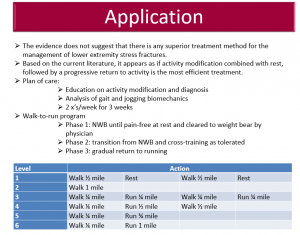
Patient will benefit from skilled aquatic physical therapy 3 times a week for 12 weeks to increase her strength, minimize exertional fatigue, decrease pain, increase hamstring, gastoc-soleus and IT band flexibility, and improve her quality of life. Aquatic physical therapy is recommended due to the fact that patient experiences increase in symptoms after too much physical activity therefore taking a slower exercise approach in a warm pool can be beneficial.
PICO: Is aquatic therapy an effective treatment option to manage physical and psychological symptoms in patients with Fibromyalgia compared to non-aquatic therapy?
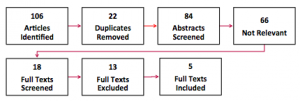
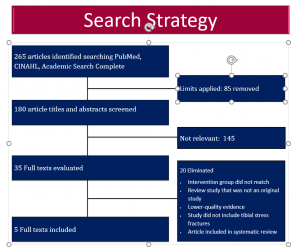
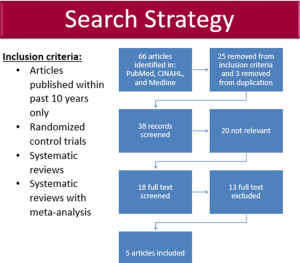
Database search: Pubmed, CINAHL, PEDro
Search Terms: “Fibromyalgia and Aquatic Therapy”
Inclusion criteria: Women with FMS; include aquatic therapy intervention and a control group; have at least one of the two outcome measures: pain and/or psychological wellbeing.
4 articles came from Pubmed and 1 article from PEDro. CINAHL had same articles as Pubmed.
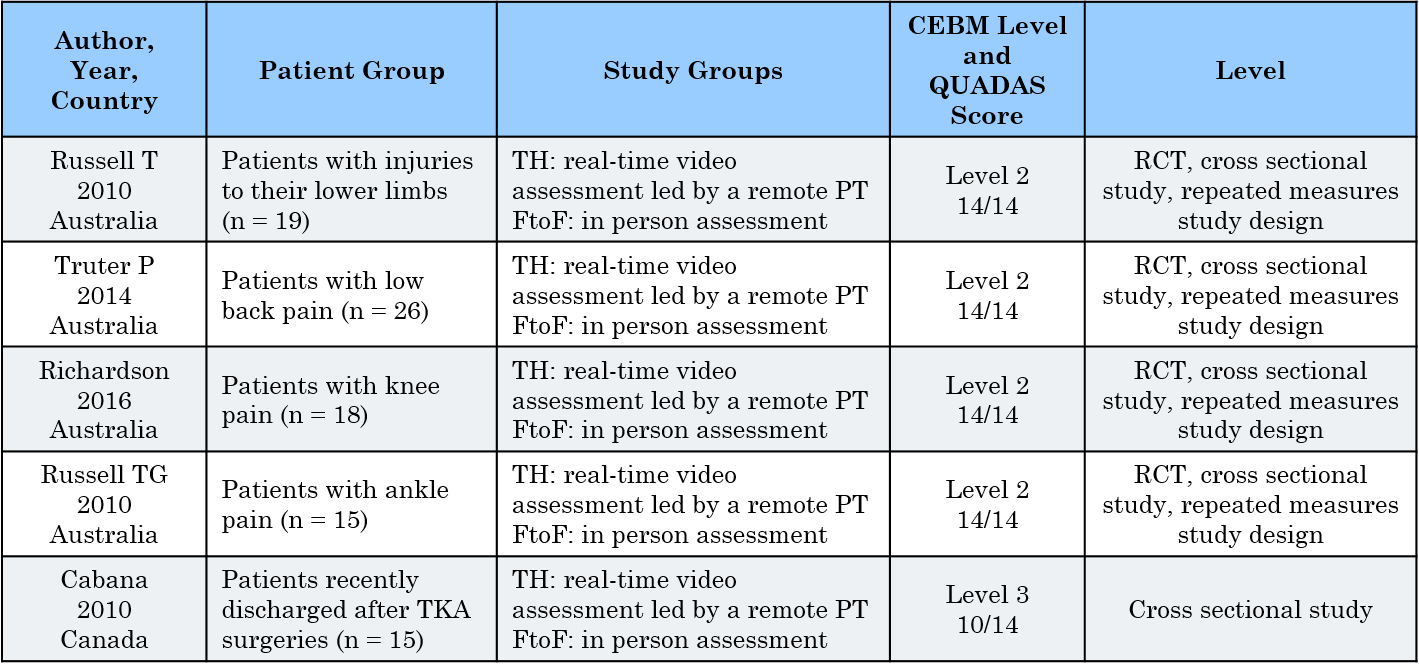
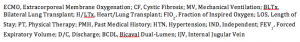
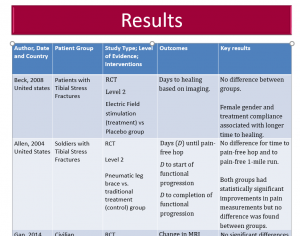
| Author Date and country: | Study Type and Level of Evidence: | Patient Group/Intervention: | Outcomes: | Key Results: | Key Results | |
| Sevimli D, 2015
Turkey |
RCT Level 2
PEDro 5/10 |
75 female patients with FMS, ages
18-50 (35+/-8.8) yrs. old |
Pain (VAS), psychological factors (BDI and MCS) | Study compared the effect of AAEP, land based AEP, and ISSP. For pain (VAS), AAEP and AEP showed significant improvements compared to ISSEP, but no significant difference between AAEP and AEP. For depression (BDI), both AAEP and AEP did significantly better then ISSEP, but AEP did better than AAEP. For the mental well being (MCS) both AAEP and AEP showed statistically significant difference but ISSEP did not, and AAEP showed more significant difference than AEP. The study suggests that AAEP has overall more benefit then AEP and ISSP in treating patients with Fibromyalgia.
|
Study compared the effect of AAEP, land based AEP, and ISSP. For pain (VAS), AAEP and AEP showed significant improvements compared to ISSEP, but no significant difference between AAEP and AEP. For depression (BDI), both AAEP and AEP did significantly better then ISSEP, but AEP did better than AAEP. For the mental well being (MCS) both AAEP and AEP showed statistically significant difference but ISSEP did not, and AAEP showed more significant difference than AEP. The study suggests that AAEP has overall more benefit then AEP and ISSP in treating patients with Fibromyalgia. | |
| Munguia-Izquierdo D, 2007, Spain | RCT Level 2
PEDro, 5/10 |
60 women (18-60 yrs. old) with FMS. 7 excluded from final results . 25 healthy individuals for comparison of FMS symptoms | Pain (VAS, and tender point count), psychological wellbeing was not evaluated in this study. | Exercise group showed significant reduction of tender point count and pain (VAS) compared to control group (with usual care). Conclusion: aquatic therapy in a warm pool can decrease pain and severity of Fibromyalgia in previously unfit women with FMS.
|
Exercise group showed significant reduction of tender point count and pain (VAS) compared to control group (with usual care). Conclusion: aquatic therapy in a warm pool can decrease pain and severity of Fibromyalgia in previously unfit women with FMS. | |
| Assis MR, 2006
Brazil |
RCT Level 2
PEDro, 8/10 |
60 sedentary women with FMS ages 18-60 years old. | Pain (VAS), Depression (BDI and FIQ), Anxiety (FIQ), and SF-36 role emotional component. | Aquatic therapy and land based therapy both showed significant improvement in pain (36% reductions in pain), but no between groups difference. For psychological well being aquatic therapy showed better results than land based therapy. Conclusion: aquatic therapy has more benefits than land based therapy for patients with Fibromyalgia.
|
Aquatic therapy and land based therapy both showed significant improvement in pain (36% reductions in pain), but no between groups difference. For psychological well being aquatic therapy showed better results than land based therapy. Conclusion: aquatic therapy has more benefits than land based therapy for patients with Fibromyalgia. | |
| Thomas-Carus P, 2008
Spain |
RCT Level 2
PEDro 6/10 |
33 Female patients with FMS, ages
37-71 yrs. old. 3 excluded from final results, 30 completed full study. |
Pain (FIQ), psychological wellbeing (depression (FIQ) and anxiety (STAI and FIQ)). | A long-lasting and regular aquatic exercise in a warm pool at moderate training intensity (60-65% HRmax) showed improvements in physical and mental health in women with FMS compared to control group. Flow-up post treatment following 8 month therapy showed benefits in anxiety status (41%), physical functioning (20%), pain management (8%), and depressive symptoms (27%).
|
A long-lasting and regular aquatic exercise in a warm pool at moderate training intensity (60-65% HRmax) showed improvements in physical and mental health in women with FMS compared to control group. Flow-up post treatment following 8 month therapy showed benefits in anxiety status (41%), physical functioning (20%), pain management (8%), and depressive symptoms (27%). | |
| Munguia-Izquierdo D, 2008
Spain |
RCT Level 2
PEDro 7/10 |
60 females with FMS (18-60 yrs. old) and 25 healthy women for symptom comparison. | Pain (tender point count), psychological (SAI) | Aquatic therapy more beneficial than usual care for pain treatment. No difference in anxiety level post treatment in both exercise and control group were found. | Aquatic therapy more beneficial than usual care for pain treatment. No difference in anxiety level post treatment in both exercise and control group were found. |
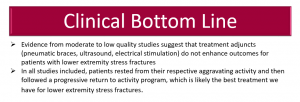
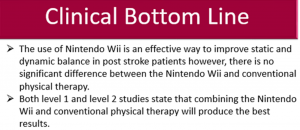
Clinical Bottom Line: Based on the research there is consistent evidence that aquatic therapy is an effective treatment option to treat pain and psychological wellbeing in patients with Fibromyalgia compared to other therapies or usual care. However, when comparing aquatic therapy to other therapies there was no significant difference between groups for pain level and better results for psychological well being favoring aquatic therapy. When comparing aquatic therapy to usual care results showed significant difference in pain and psychological wellbeing favoring aquatic therapy.
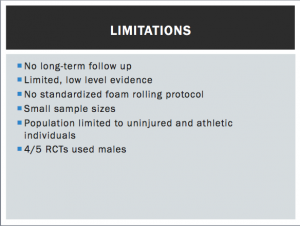
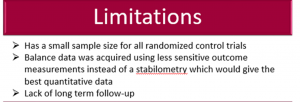
Limitations: Small sample size. No blinding of the subjects, assessors or therapist. Only one study had blinding of the assessors. All five RCTs were done outside of the United States. Short therapy duration. Only one study was long term. A future need for longer term studies considering chronic nature of FMS.
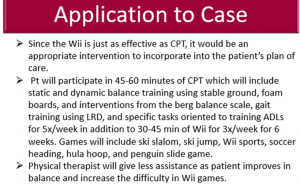
Application of the evidence to case scenario: Aquatic therapy 2 times per week for 8 weeks. Progress to once a week aquatic therapy and once a week land based therapy for manual stretching and advanced strengthening exercises. Continue with aquatic therapy at least once a week for psychological well being, pain, and fatigue symptoms.
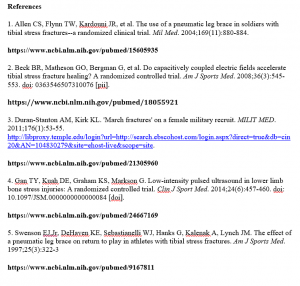
References:
- Sevimli D, Kozanoglu E, Guzel R, Doganay A. The effects of aquatic, isometric strength-stretching and aerobic exercise on physical and psychological parameters of female patients with fibromyalgia syndrome. J Phys Ther Sci. 2015 Jun;27(6):1781-6. doi: 10.1589/jpts.27.1781. Epub 2015 Jun 30. PubMed PMID: 26180320; PubMed Central PMCID: PMC4499983.
- Munguía-Izquierdo D, Legaz-Arrese A. Exercise in warm water decreases pain and improves cognitive function in middle-aged women with fibromyalgia. Clin Exp Rheumatol. 2007 Nov-Dec;25(6):823-30. PubMed PMID: 18173915
- Munguía-Izquierdo D, Legaz-Arrese A. Assessment of the effects of aquatic therapy on global symptomatology in patients with fibromyalgia syndrome: a randomized controlled trial. Arch Phys Med Rehabil. 2008 Dec;89(12):2250-7. doi: 10.1016/j.apmr.2008.03.026. PubMed PMID: 19061736.
- Assis MR, Silva LE, Alves AM, Pessanha AP, Valim V, Feldman D, Neto TL, Natour J. A randomized controlled trial of deep water running: clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis Rheum. 2006 Feb 15;55(1):57-65. PubMed PMID: 16463414.
- Tomas-Carus P, Gusi N, Häkkinen A, Häkkinen K, Leal A, Ortega-Alonso A. Eight months of physical training in warm water improves physical and mental health in women with fibromyalgia: a randomized controlled trial. J Rehabil Med. 2008 Apr;40(4):248-52. doi: 10.2340/16501977-0168. PubMed PMID: 18382819.

 TH: telehealth; FtoF: face-to-face
TH: telehealth; FtoF: face-to-face







 4
4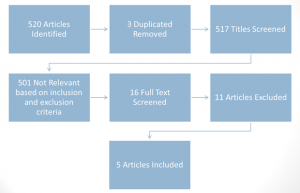
 2
2 4
4 4
4