Background:
There are ~4 million ICU admissions per year with an average mortality rate of 8-19%, or about 500,000 deaths annually. These patients are at high risk for adverse outcomes due the severity of illness and the multiple and complex interventions given to them at the same time. “Critical care is a costly component of the national health care budget, with costs estimated to be $81.7 billion…These costs are largely explained by the length of stay (LOS) in the ICU”.1
Case Scenario:
Mr. B, a 78-year-old male, went into cardiac arrest while on a morning jog and was resuscitated via CPR by a Good Samaritan. He underwent a coronary artery bypass graft (CABG) after it was discovered that he suffered a myocardial infarction. He has been sedated and mechanically ventilated for the past 48 hours in the ICU and the physician lets you know he will be coming off of sedation today. Mr. B has a limited PMH and vitals are stable and safe for mobility at this time
Clinical Question:
In patients who are mechanically ventilated >24 hours, is early mobilization effective in significantly reducing the amount of time spent in the ICU?
Search Strategy and Results:
A literature search was performed to identify eligible randomized controlled trials (RCT), clinical trials, cohort studies and single-blind studies. Electronic searches of MEDLINE, CINAHL, and PUBMED using the key words “physical therapy” or “early mobilization” or “rehabilitation” and “ICU” or “critical care” and “mechanical ventilation” and “length of stay” were conducted. Only full reports in English were included. Inclusion criteria were as follows: Design: RCT, clinical trial, cohort study or single blind studies; Participants: Ages 19+, male or female, >24 hours on mechanical ventilation, patients in the ICU; Interventions: early mobilization or physical therapy including active or passive exercises in bed, side of bed, and/or ambulation, once or twice a day; Comparisons: usual care, delayed mobilization, as ordered by physician; Outcomes: ICU length of stay, ICU-acquired weakness (ICUAW) and adverse events.

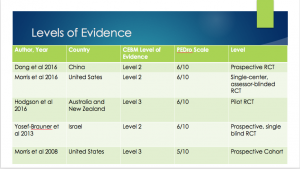
Evidence Appraisal:
Evidence Summary:
| Author Date and Country | Patient Group | Outcomes | Key Results |
| Dong
2016 China
|
106 patients who underwent CABG between June 2012 and May 2015 in the ICU of the Affiliated Hospital of Qingdoa University, requiring >72 hours of mechanical ventilation were randomly assigned to:
Early rehab group: (n=53) Control group: (n=53)
|
ICU length of stay
|
There were no significant differences in basic characteristics between groups at baseline (P>0.05).
Patients in early rehabilitation groups had significantly shorter duration of ICU stay (early rehab group: 11.7+/-3.2 days; control: 18.3+/-4.2days, P<0.01 Duration of mechanical ventilation was significantly reduced (early rehab group: 8.1+/-3.3 days; control: 13.9+/-4.1 days, p<0.01 Hospital length of stay was significantly reduced (early rehab group: 22.0+/-3.8 days; control: 29.1+/-4.6 days, p<0.01 |
| Morris
2016 United States |
300 adult patients admitted to the ICU at Wake Forest Baptist Medical Center, NC with acute respiratory failure requiring mechanical ventilation were randomized to:
Standard Rehabilitation Therapy (SRT)= (n=150) Usual care= (n=150) |
ICU days
|
No significant difference in duration of ICU days. Median (IQR); SRT= 7.5 (4 to 14); usual care=8.0 (4 to 13); p=0.68
No difference in adverse event reporting between groups. |
| Hodgson
2016 Australia and New Zealand |
50 critically-ill adults mechanically ventilated for >24 hours randomly assigned to:
Early goal-directed mobilization(EGDM), intervention: (n=29) Standard care, control: (n=21) |
ICU length of stay
ICU-acquired weakness
|
There was in imbalance at baseline with respect to age, with intervention patients begin older than control patients.
There were no serious adverse events reported that occurred in conjunction with an episode of EGDM. The proportion of patients who walked in the ICU was almost doubled with EGDM (intervention, n=19 (66%) versus control, n=18 (38%), p=0.05. No significant difference was found between groups regarding ICU length of stay: EGDM= 9 (6-17); control=11 (8-19), p=0.28. No significant difference in ICU acquired weakness was found between group at hospital discharge, p=0.13 |
| Yosef-Brauner
2013 Israel |
18 patients admitted to the ICU at Kaplan Medical Center and who required mechanical ventilation >48 hours were randomly divided into two intervention groups:
Control Group: (n=9) Intensive group: (n=9) |
ICU length of stay | At baseline, there were no significant differences in the demographic and clinical characteristics between the groups.
A statistically significant difference was found in the number of ICU days between groups: LOS in group 1= 18.11+/-3.1 days and group 2= 13+/-4.6 days, (P=0.043).
|
| Morris
2008 United States |
330 patients in the ICU with acute respiratory failure requiring mechanical ventilation- ID’d prospectively and enrolled in the study within 48 hours of intubation and 72 hours of admission to ICU.
Usual care: (n=165) Protocol: (n=165)
|
ICU length of stay
|
There were no significant differences at baseline between the protocol and usual care group.
The adjusted ICU LOS for the Usual Care group was 6.9 days vs. the Protocol group 5.5 days, (p=0 .027) No adverse events during ICU mobility. |
Clinical Bottom Line:
There is mixed and lower-quality evidence suggesting that early mobilization can significantly reduce the ICU length of stay
There were no significant adverse events reported in any of these studies suggesting that early mobilization in these patients is safe and feasible.
Application of the Evidence:
The clinician needs to consider the patient’s prior level of function, goals, expectations and level of motivation. They also need to consider if the entire mobility team is on board including (but not limited to) the ICU nurse, physician, physical therapist, occupational therapist and respiratory therapist. In this particular case, Mr. B was previously very active and independent and is currently highly motivated to return home with his wife and eventually run again. The entire mobility team is also on board at this time. Due to Mr. B’s prior level of activity, we are choosing to implement the “Early Goal-Directed Mobilization” (EGDM) protocol 7 days per week at the level determined by the ICU Mobility Scale (which is outside the realm of this research). The EGDM protocol was used in the Hodgson et al 2016 study (as shown below):
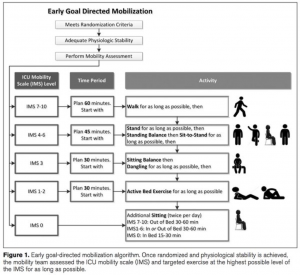
https://twitter.com/iwashyna/status/717023531503058944
References:
1. ICU outcomes (mortality and length of stay) methods, data collection tool and data. Philip R. Lee Institute for Health Policy Studies Web site. http://healthpolicy.ucsf.edu/content/icu-outcomes#ICU%20BACKGROUND. Accessed 09/23, 2016.
2. Dong Z, Yu B, Zhang Q, et al. Early rehabilitation therapy is beneficial for patients with prolonged mechanical ventilation after coronary artery bypass surgery. Int Heart J. 2016;57(2):241-246. doi: 10.1536/ihj.15-316 [doi].
3. Morris PE. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: A randomized clinical trial. JAMA : the Journal of the American Medical Association. 06;315(24):2694; 2694-2702; 2702.
4. Hodgson CL, Bailey M, Bellomo R, et al. A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med. 2016;44(6):1145-1152. doi: 10.1097/CCM.0000000000001643 [doi].
5. Yosef-Brauner O, Adi N, Ben Shahar T, Yehezkel E, Carmeli E. Effect of physical therapy on muscle strength, respiratory muscles and functional parameters in patients with intensive care unit-acquired weakness. Clin Respir J. 2015;9(1):1-6. doi: 10.1111/crj.12091 [doi].
6. Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238-2243. doi: 10.1097/CCM.0b013e318180b90e [doi].
Contact Andrea Dietrich at Andrea.Dietrich@temple.edu for further information.