Background
- Cerebral Palsy (CP) is the most common motor disability in children.1
- 1986 Congress established the early intervention program for infants and toddlers with disabilities, as part of the Individuals with Disabilities Education Act (IDEA).2
- “IDEA Part C states that infants and toddlers with disabilities receive needed early intervention services in the natural environments to the maximum extent appropriate.”2
- May be provided in other settings only when the services cannot be achieved satisfactorily in a natural environment.2
- “According to the Data Accountability Center, in 2011, a total of 336,895 eligible infants and toddlers birth through age 2 received early intervention services under Part C of IDEA.”2
Clinical Scenario
- 15 month old male with recent diagnosis of spastic diplegic Cerebral Palsy
- Born via C-Section at 32 weeks with initial Apgar score of 2
- 4th degree intraventricular hemorrhage at 2 weeks
- Unable to sit up on his own
- Maintains ATNR & TLR Reflexes
- No righting responses
- Peabody Developmental Motor Scale: 45 (“very poor”)
- Goal: sit independently and introduce quadruped
PICO
- What are the effects of early intervention on motor function in children who have, or are at a high risk of developing cerebral palsy?
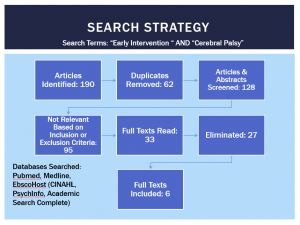
Search Strategy
Results
Hielkema et. Al, 20113
- RCT, CEBM Level 2, PEDro 9/11; Netherlands
- Participants
- 46 patients, corrected age 3 months with abnormal general movements at 10 weeks of age
- Intervention (3 month minimum; then varied)
- COPCA (COPing and Caring for Infants with Special Needs)
- TIP (Traditional Infant Physiotherapy)
- Outcome Measure
- Infant Motor Profile (IMP)
- Results
- No statistical difference between groups
- Self-produced movement behavior with little variation has positive correlation
Morgan et. Al, 20154
- Pilot RCT, CEBM Level 3, PEDro 9/11; Australia
- Population
- 13 infants, corrected age 3-5 months with abnormal general movements between 11-18 weeks
- Intervention (3 months)
- GAME (Goal- Activity- Motor Enrichment)
- GAME Intervention- Focuses on goal oriented intensive motor training in which the infant can always actively complete part of the task.
- Parent Education to identify when a child is voluntarily trying to move, how to stimulate progress and identify naturally occurring opportunities for learning.
- Environment Enrichment- setting up an environment to stimulate movement and matching the toy selection to the desired task.
- Standard Care (Movement patterns & parental advice on positioning & handling)
- GAME (Goal- Activity- Motor Enrichment)
- Outcome Measure
- PDMS-2 (Peabody Developmental Motor Scale 2)
- Results
- Total Motor Quotient (TMQ) & the Total Motor Subscale of Peabody both statistically significant over the standard care group
- GAME intervention had an 8.05 point improvement in TMQ and a 5.72 advantage improvement in total motor subscale over the standard care group.
- Post hoc analysis- significant difference between groups in number of hours of therapy time and HEP time. GAME group received an average of 9.93 hours and the SC group received 3.49 (this could also account for the differences between groups outcome scores)
- Total Motor Quotient (TMQ) & the Total Motor Subscale of Peabody both statistically significant over the standard care group
Morgan et. Al, 20165
- RCT, CEBM Level 2, PEDro 7/11; Australia
- Population
- 30 infants, corrected age 3-4 months with abnormal general movements or 5-6 months with CP diagnosis or abnormal neuroimaging resulting in CP diagnosis extremely likely
- Intervention (Until 1 y.o)
- GAME (Goal-Activity- Motor Enrichment)
- Standard Care (milestone attainment directed)
- Outcome Measure
- PDMS-2 (Subscale- Total Motor Quotient)
- GMFM (Gross Motor Function Measure)
- Results
- All outcome measures were statistically significant in favor of the GAME intervention group
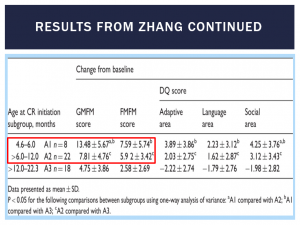
Zhang et. Al, 20156
- Longitudinal Cohort, CEBM Level 3, Downs & Black 19/27; China
- Population
- 48 infants (Under 2 years of age) with a confirmed diagnosis of CP
- Intervention (3 months)
- Comprehensive Rehab
- Comprehensive Rehab consisted of PT, OT, Speech, and multiple alternative medicine approaches
- Outcome Measure
- GMFM
- FMFM (Fine Motor Function Measure)
- Results
- Greater improvements and more statistical significance seen when initiated before 12 months of age
- Comprehensive Rehab
Mahoney et. Al, 20017
- Field Based Study, CEBM Level 3, Downs & Black 18/27; USA
- Population
- 50 infants, average age of 14 months; 23 with CP & 27 with DS
- Intervention (1 Year, Apx. 40 sessions)
- DevS (Developmental Skills)
- 5 Developmental skills sites- comprehensive early intervention service programs with 45% having physical therapy training.
- NDT (Neuro-Developmental Treatment)
- 4 NDT Sites– 3 hospital based, 1 comprehensive center-based early intervention program- children with motor disabilities– 77% of PTs at NDT sites were NDT certified
- Outcome Measure
- PDMS-2
- Results
- No statistical significance in PDMS scores
- Unable to determine if the improved scores are due to treatment or the natural growth and development over a 1 year period.
- No statistical significance in PDMS scores
- DevS (Developmental Skills)
Heathcock et. Al, 20158
- Case Series, CEBM Level 4, Downs & Black 14/27; USA
- Population
- 2 infants with spastic quadriplegic CP, GMFCS Level 5
- Intervention (4 weeks)
- 2 hours/day for 5days/week for 4 consecutive weeks- 40 hours total
- Outpatient therapist-directed PT treatment
- Developmental positioning and anti-gravity movement
- Outcome Measure
- GMFM- 66
- GMFM-88
- Results
- Clinically meaningful change for both children in both outcome measures
- Clinically Meaningful Change: GMFM- 66- 1.58 points; GMFM-88- 1.29 points
- Child A- GMFM- 66 score improved by 6.06 and GMFM-88 improved by 12 points
- Child B- GMFM-66 scores improved by 9.3 and GMFM-88 improved by 16 points
- Family & Therapist goals were met
- Clinically meaningful change for both children in both outcome measures
Limitations
- Only 2 studies with similar interventions
- Experimental interventions were not standardized or explained in detail
- Lack of description of the standard care groups (control group)
- Small samples sizes
- Minimal to no description of intervention dosage
- Relatively short time frames for the length of the studies
- Lack of studies which are CEBM levels 1 & 2
Clinical Bottom Line
- The evidence shows that beginning early intervention PT before 1 year old has increased improvements for motor performance in children with, or are at a high risk of developing CP.
- There is insufficient evidence as to what form of physical therapy intervention is superior and what the correct dosage should be.
- However, the lower quality studies included suggest high intensity is correlated with increased improvements.
Application to Case
- Multifactorial
- Use aspects of GAME intervention with basic motor control and motor development patterns
- Goal oriented
- Sitting with support à sitting independently
- Rolling with time spent on his belly
- Initiating quadruped
- Parent education and involvement
- High intensity recommended with PT 4x/week
- Extensive HEP
Acknowledgements
- Thank you Dr. Richard Lauer and Class of 2017!
References
- 1. Data & Statistics for Cerebral Palsy. Centers for Disease Control and Prevention. http://www.cdc.gov/ncbddd/cp/data.html. Published February 2016. Accessed October 2, 2016.
- 2. Center for Parent Information and Resources. Center for Parent Information and Resources. http://www.parentcenterhub.org/repository/ei-history/. Accessed October 2, 2016.
- 3. Hielkema T, Blauw-Hospers CH, Dirks T, Drijver-Messelink M, Bos AF, Hadders-Algra M. Does physiotherapeutic intervention affect motor outcome in high-risk infants? An approach combining a randomized controlled trial and process evaluation. Dev Med Child Neurol. 2011 Mar;53(3):e8-15. doi: 10.1111/j.1469-8749.2010.03876.x. PubMed PMID: 21291457.
- 4. Morgan C, Novak I, Dale RC, Badawi N. Optimising motor learning in infants at high risk of cerebral palsy: a pilot study. BMC Pediatr. 2015 Apr 1;15:30. doi: 10.1186/s12887-015-0347-2. PubMed PMID: 25880227; PubMed Central PMCID: PMC4389951.
- 5. Morgan C, Novak I, Dale RC, Guzzetta A, Badawi N. Single blind randomised controlled trial of GAME (Goals—Activity—Motor enrichment) in infants at high risk of cerebral palsy. Res Dev Disabil. 2016;55:256-267. http://libproxy.temple.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2016-37412-024&site=ehost-live&scope=site. doi: 10.1016/j.ridd.2016.04.005.
- 6. Zhang H, Zhang B, Jia F, et al. The effects of motor and intellectual functions on the effectiveness of comprehensive rehabilitation in young children with cerebral palsy. J Int Med Res. 2015;43(1):125-138.