Background:
- More than 795,000 people suffer from a cerebral vascular accident (CVA) each year
- Ischemic strokes account for approximately 87% of all CVA’s
- Leading cause of disability in the United States
- CVA’s cost an estimated $34 billion each year
- Includes medication costs, health care services, and missed work days
- Repetitive Transcranial Magnetic Stimulation (rTMS) is a device that uses an electromagnet to stimulate small areas of the brain
- This is achieved by low or high frequency magnetic pulses that send an electric current across the brain tissue
- Low frequency stimulation has inhibitory effects
- Transcallosal Disinhibition: By inhibiting the non-lesioned hemisphere the theory is that competition between hemispheres is decreased and it allows for more cortical excitability due to the non-lesioned hemisphere no longer inhibiting the affected hemisphere.
- High frequency stimulation has excitatory effects

Image source: www.practicalpainmanagement.com
Case Scenario:
- Hank is a 66 y.o. male diagnosed with a left middle cerebral artery thrombotic infarction 2 weeks ago. He underwent surgery for recanalization of his left MCA and was placed on anticoagulants. Hank has a past medical history of hypertension, diabetes mellitus II, and peripheral vascular disease.
Upon exam Hank was A&O x 3, able to follow commands, and provide social history. He is a retired school teacher who enjoys working on antique cars in his free time. Hank lives at home in a 1 story house with his wife and was previously independent with all ADLs and IADLs. He denies any pain but states, “I just can’t really feel my left hand very well.” Hank is 6’1” and 182 lbs and right hand dominant.
Hank is very hopeful that PT will “get his arm moving like it used to” so he has the upper extremity strength and hand dexterity to continue working on his cars.
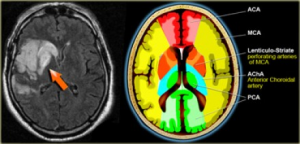
Image Source: www.radiologyassistant.nl
Key Exam Findings:
- Right upper extremity demonstrates a flexion synergy pattern with AROM
- Manual muscle tests of the right upper extremity
- Shoulder flexion 3/5
- Elbow flexion 2/5
- Elbow extension 2/5
- Decreased grip strength
- Diminished sensation to light touch in right upper extremity throughout C6-T1 dermatomes
PICO Question:
Does repetitive transcranial magnetic stimulation before activity training enhance upper extremity motor recovery in adults s/p CVA?
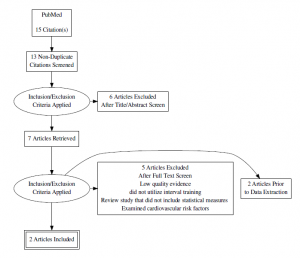
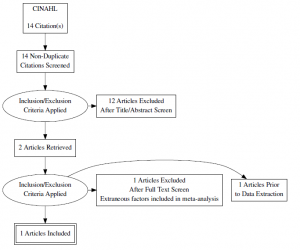
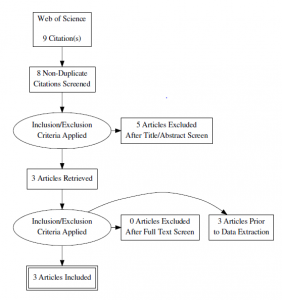
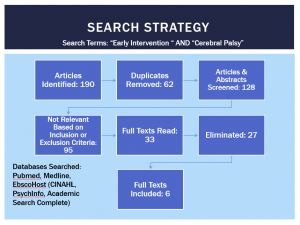
Search Strategy:
The following limits were applied: Published within the past 10 years, human species, English language, Meta-analyses, Systematic Reviews, RCTs
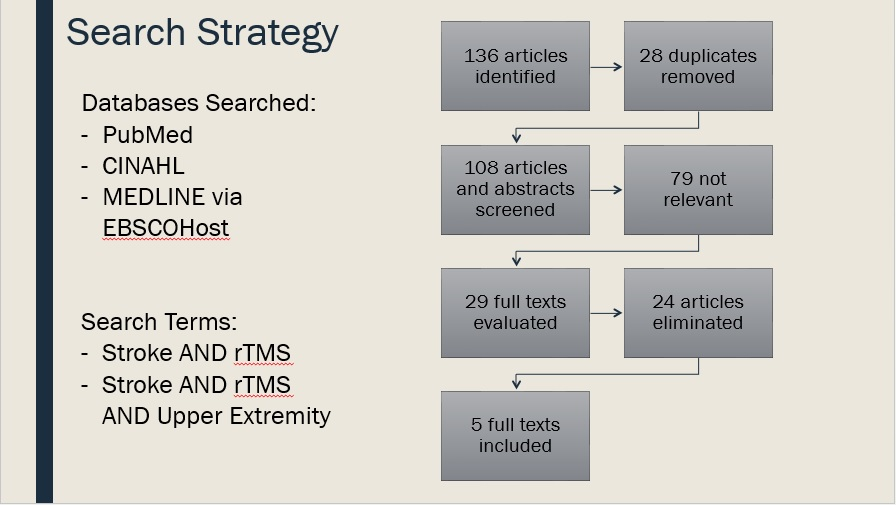
Inclusion Criteria, article must include:
- Adults (>18 years old) who present with upper extremity paresis after stroke
- At least one intervention arm that consisted of repetitive transcranial magnetic stimulation to either the ipsilesional or contralesional hemisphere
- At least one intervention arm that consisted of motor/activity training after stimulation
- Assessment of at least one of the following outcome measures:
- Fugl- Meyer Assessment
- Wolf Motor Function Test
- 9 Hole Peg Test
- Grip strength
- Upper limb force production
Exclusion Criteria, article cannot include:
- Stimulation to areas of the brain other than M1 or the premotor cortex
- Other non-invasive brain stimulation techniques
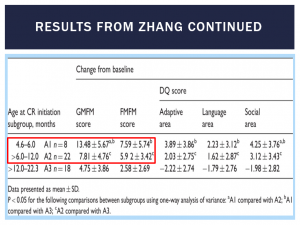
Evidence Summary Table:
| Author, Date, and Country | Patient Population | Study Type and Level of Evidence | Outcomes | Conclusion | Study Weaknesses |
| Hao, 2013
China |
Patients of any age or sex after stroke, regardless of the duration of illness or severity of the initial impairment | Systematic Review
Level I PRISMA: 23/27 |
Motor Outcomes: Jebsen-Taylor Hand Function Test, Pegboard Task, Wolf Motor Function Test, Action Research Arm Test | –Use of rTMS for patients with stroke is not recommended until its efficacy is verified in high-quality, large scale RCT’s
–Subgroup analysis: Contralesional rTMS displayed a moderate effect size on motor outcomes |
Small number of subjects across all articles reviewed with sample sizes ranging from 10 to 123.
Stimulation parameters varied across studies. No studies included with long term follow-up. Inclusion criteria for participants was not very strict, for example a study with pediatric patients was included. Meta-Analysis for motor function was only performed on 4 of 19 studies.
|
| Hsu, 2012
Taiwan |
Adults diagnosed with stroke | Systematic Review
Level I PRISMA: 20/27 |
Wolf Motor Function Test, Nine-Hole Peg Test, Grip Strength |
–rTMS suggests a clinically positive effect on motor recovery in the affected upper limb of patients with stroke –Low frequency rTMS over the contralesional hemisphere being more effective in enhancing upper limb motor recovery based on subgroup analysis |
Small number of subjects across all articles reviewed
Many articles reviewed report a wide variety of long term outcomes, if any (from 2 weeks to 1 year), Outcome measures, experimental designs, inclusion criteria, and rTMS protocols varied between articles.
|
| Etoh, 2013
Japan |
Adults with chronic stroke; either first or second unilateral stroke | Randomized Double-Blind Crossover Study
Level II PEDro: 6/10 |
Fugl-Meyer Assessment, Action Research Arm Test, Simple Test for Evaluating Hand Function | –Low frequency inhibitory rTMS to the contralesional hemisphere facilitated the effects of repetitive facilitation exercises (100 reps of 5 to 8 exercises) in improving the motor function of the affected upper limb in patients with chronic stroke | Very small sample size.
“Sham” stimulation still involved actual use of the rTMS coil and it is possible that there was some stimulation to the motor cortex or the sensory cortex that may have confounded the results. No long term follow-up. Generalizability limited to those with unilateral chronic stroke
|
| Seniow, 2012
Poland |
Adults diagnosed with stroke with onset of symptoms <3months | Randomized Control Trial Level II PEDro: 9/10 |
Fugl-Meyer Assessment, Wolf Motor Function Test |
Contralesional inhibitory stimulation to the primary motor cortex by low frequency rTMS is not yet an evidence-based method during early rehab for patients with stroke There were statistically significant differences in both groups from pre test to post test scores, however there were no significant between group differences
|
Small sample size, The article stated that those in the experimental group received more PT posttreatment, There was loss to follow-up in both groups potentially skewing the data, though an intention to treat analysis was performed.
Generalizability limited to those in early rehabilitation post stroke |
| Wang, 2014
Taiwan |
Adults with chronic stroke | Randomized Control Trial
Level II PEDro: 9/10 |
Fugl-Meyer Assessment, Wolf Motor Function Test, Medical Research Council Scale (grip strength and shoulder flexion) | Inhibitory rTMS to the contralesional premotor cortex or primary motor cortex facilitated restoration of motor function in patients with chronic stroke
The patients assigned to the contralesional M1 and contralesional dorsal premotor cortex groups showed significant improvements in MRC, FMA, and WMFT scores post-rTMS compared with those of the sham group, with stimulation to M1 demonstrating larger effect sizes than stimulation to the dorsal premotor cortex.
|
Small sample size with a very homogeneous sample of only right handed patients and those with an MCA infarct – not very generalizable. There was no control group for the premotor cortex stimulation. Stimulation to the dorsal premotor cortex was only 3 cm away from the M1 stimulation area, while simultaneously stimulating M1 was attempted to be controlled there may have been some overlap.
Generalizability limited to those with chronic stroke.
|
Clinical Bottom Line:
There is moderate to high-quality evidence that suggests low frequency, inhibitory repetitive magnetic transcranial stimulation (rTMS) to the contralesional hemisphere may be an effective intervention in facilitating upper extremity motor recovery in those with chronic stroke. However, more research is needed to determine this treatments effectiveness in other stroke populations.
rTMS is an emerging intervention in stroke rehabilitation, and the current evidence varies greatly in terms of acuity of stroke, type of stimulation administered, hemisphere stimulated, and type of motor training performed after rTMS intervention. These variations across studies made it more difficult to draw a consistent conclusion from all articles reviewed.
Application to Case Scenario:
- The literature does not suggest that rTMS will have a significant effect on the patient in my case scenario based on the acuity of his stroke as he is 2 weeks s/p CVA.
- POC for my patient:
- Interventions will include:
- Weight bearing exercises through the affected upper extremity
- Reaching tasks
- Active assisted range of motion exercises
- Goal of progressing to strength training and fine motor skill training
- Interventions will include:
- Discharge plan for outpatient PT
- POC for my patient:
Acknowledgements: Dr. Richard Lauer, PhD
References:
1. Hao Z, Wang D, Zeng Y, Liu M. Repetitive transcranial magnetic stimulation for improving function after stroke. Cochrane Database Syst Rev. 2013;(5):CD008862.
2. Hsu WY, Cheng CH, Liao KK, Lee IH, Lin YY. Effects of repetitive transcranial magnetic stimulation on motor functions in patients with stroke: a meta-analysis. Stroke. 2012;43(7):1849-57.
3. Etoh S, Noma T, Ikeda K, et al. Effects of repetitive trascranial magnetic stimulation on repetitive facilitation exercises of the hemiplegic hand in chronic stroke patients. J Rehabil Med. 2013;45(9):843-7.
4. Seniów J, Bilik M, Leśniak M, Waldowski K, Iwański S, Członkowska A. Transcranial magnetic stimulation combined with physiotherapy in rehabilitation of poststroke hemiparesis: a randomized, double-blind, placebo-controlled study. Neurorehabil Neural Repair. 2012;26(9):1072-9.
5. Wang CC, Wang CP, Tsai PY, Hsieh CY, Chan RC, Yeh SC. Inhibitory repetitive transcranial magnetic stimulation of the contralesional premotor and primary motor cortices facilitate poststroke motor recovery. Restor Neurol Neurosci. 2014;32(6):825-35.
For further questions please contact: brooke.walters@temple.edu