Research Performed by: Cara Fowler, SPT
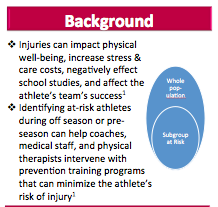
Background:
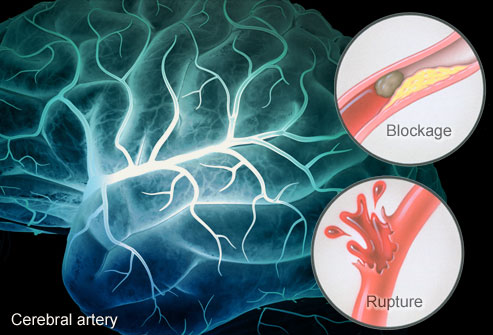
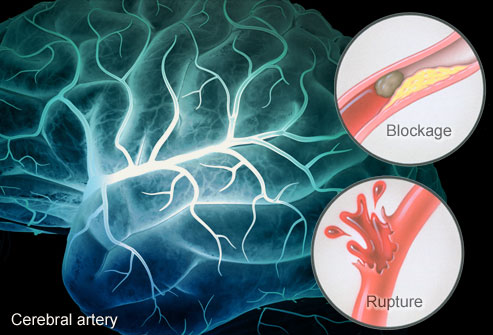
Obtained from: http://img.webmd.com/dtmcms/live/webmd/consumer_assets/site_images/articles/health_tools/stroke_overview_slideshow/webmd_rm_illustration_of_stroke_causes_.jpg
Stroke is the number one cause of long-term disability in the United States.¹ Eight out of ten stroke survivors suffer from residual hemiparesis that results in a multitude of impairments including decreased balance, gait ability, and coordination.² Dynamic balance and gait dysfunction are the two prevalent impairments in individual’s post-hemiparetic stroke and place individuals at a higher risk of falling and results in impaired functional mobility.²
Virtual reality is a form of interactive simulation that immerses patient’s within a virtual environment that gives patient’s similar experiences to real-world events within a safe and controllable clinical environment.³ Virtual reality has been explored in the chronic stroke population to improve stroke outcomes in many aspects, including balance and gait.3-7 Virtual reality has been theorized to increase patient’s motivation and adherence in a physical therapy program.³ Virtual reality also provides users with the ability to receive real time feedback based on their performances, increasing their knowledge of performance leading to more improvements in their performance.³ For these reasons, it may be a feasible option to integrate wishing a conventional physical therapy regimen in order to promote better outcomes.
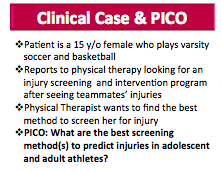
Clinical Scenario:
Mrs. Anita Cooke is a 65-year-old female that is presenting to physical therapy with the chief complaint of right-sided weakness, primarily in her lower extremity, after suffering from a Left Anterior Cerebral Artery Stroke 12-months ago. For the two years prior to her stroke, Anita was enjoying her retirement from being a school teacher by going for daily walks around her neighborhood, watching her granddaughter three times per week, taking care of her home, and playing video games with her grandson. Prior to her stroke, Anita was independent in all ADLs and IADLs. Anita’s goals are to: 1) return to her prior level of function, 2) play with her granddaughter again, 3) improve her balance, 4) go for walks around her neighborhood again, and 5) increase her confidence in her ability to move around.
Anita’s physical therapy exam revealed that she had normal active and passive range of motion in her upper and lower extremities, normal cognition (as demonstrated by score of 25 on the MMSE), difficulty isolating movements in her right lower extremity, decreased dynamic balance, and decreased walking abilities. More specifically, Mrs. Cooke ambulated independently with a single point cane and asymmetric gait pattern with decreased cadence, decreased right foot clearance, and decreased step length with left lower extremity. Anita completed the following functional tests and measures with the corresponding scores:
- Timed Up and Go: 20 seconds with single point cane (patient had difficulty with sit to stand transfer and ambulated slowly) and 35 seconds with no Assistive Device
- Berg Balance Scale: 40/56
- 10-Meter Walk Test: gait speed = 0.5 m/s
- 6-Minute Walk Test: 50m with 5 rests of 15 seconds
- ABC Scale: 70
Clinical Question:
In adult patients (> 18 years old) with chronic stroke resulting in hemiparesis, are virtual reality (VR) interventions in addition to conventional physical therapy (CPT) more effective than CPT alone in improving dynamic balance and gait outcomes?
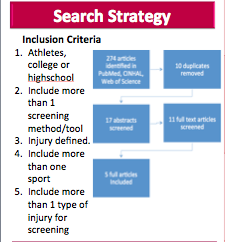
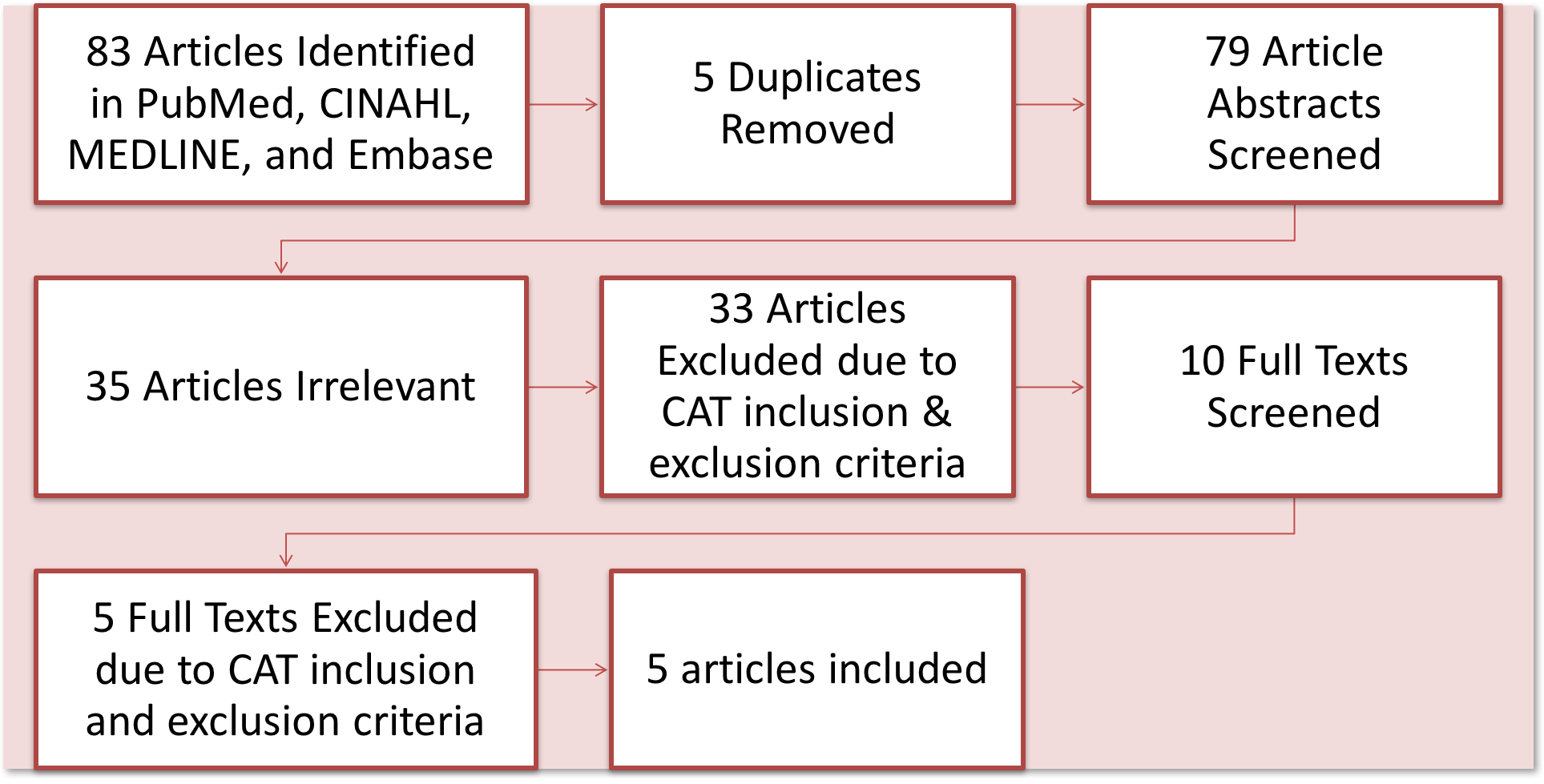
Search Strategy:
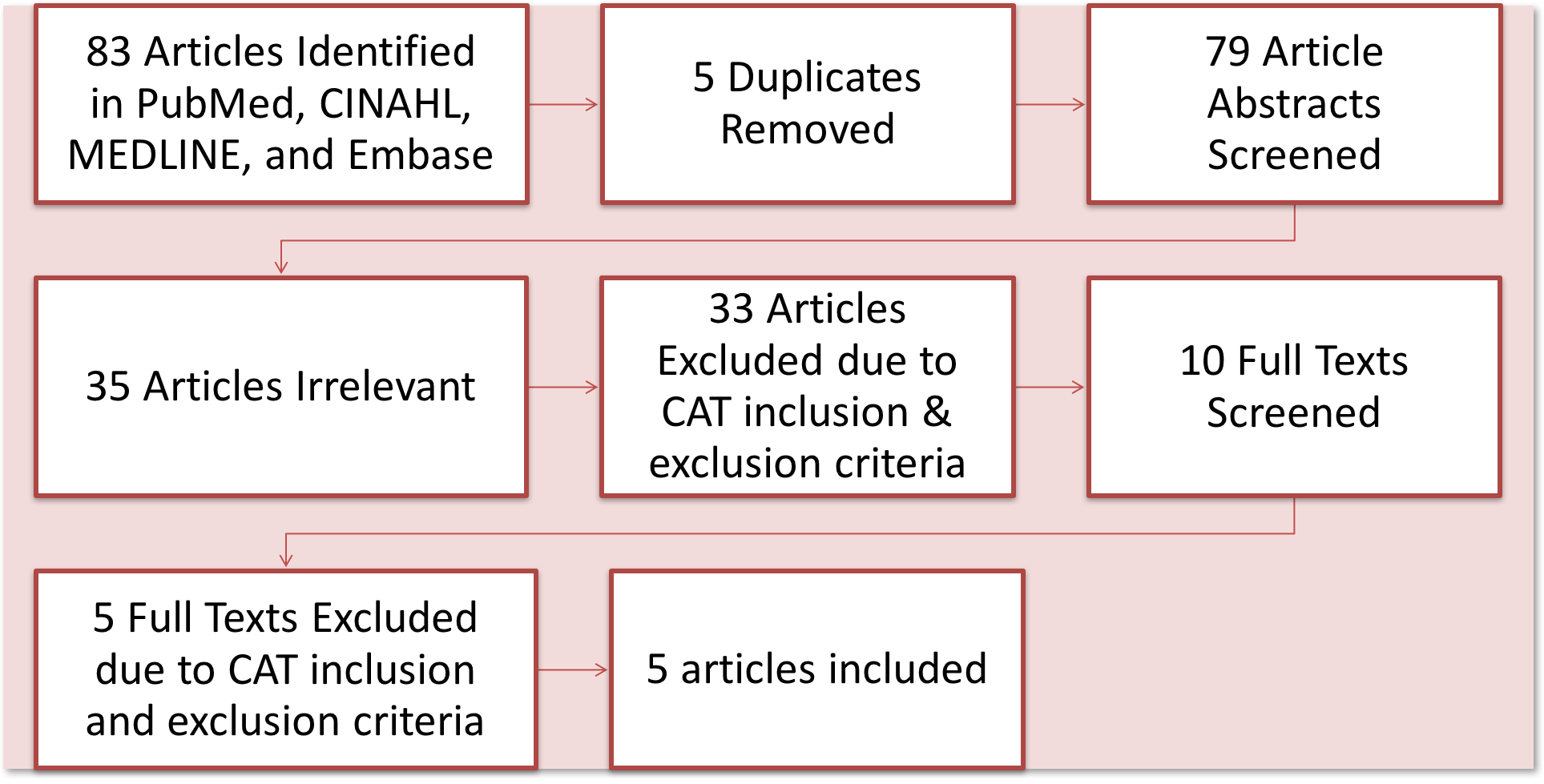
A literature search was performed to identify all eligible randomized controlled trials. Electronic searches of PubMed, CINAHL, Embase, and MEDLINE was performed using the keywords ‘stroke’ or ‘chronic stroke’; and ‘balance’, ‘postural balance’, or ‘berg balance’; and ‘virtual reality’. Only full reports in English were included. On the basis of titles and abstracts, articles were determined relevant or irrelevant. The inclusion criteria were as follows: articles published within the last 10-years; Design – RCT; Participants – Adults age > 18, male or female, with chronic stroke (> 6 months) resulting in hemiparesis; Outcomes – Berg Balance Scale (BBS), Timed up and go (TUG), 10-m walk test (10MWT); Comparison – Conventional or standard rehabilitation; Intervention – intervention with virtual reality and conventional or standard rehabilitation. Pilot studies, systematic reviews, and meta analyses were excluded. Additional studies were excluded if they utilized Telerehabilitation in the home environment, video game consoles (Wii, Wii Balance Board, PlayStation, Xbox Kinnect, etc.) as virtual reality, and studies with acute or subacute stroke participants. These inclusion and exclusion criteria resulted in 5 papers being included in this review.
Results:
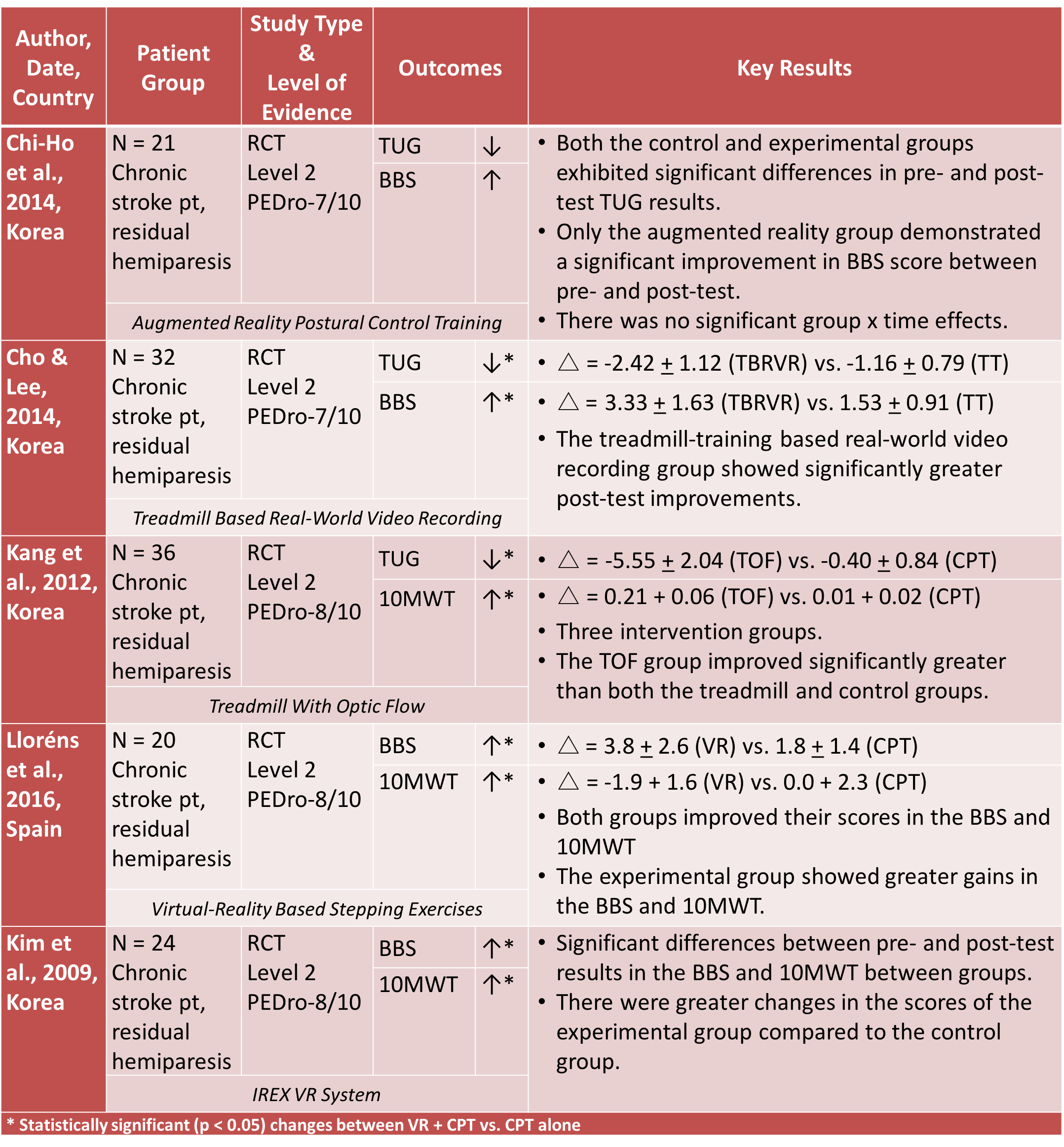
Evidence Summary:
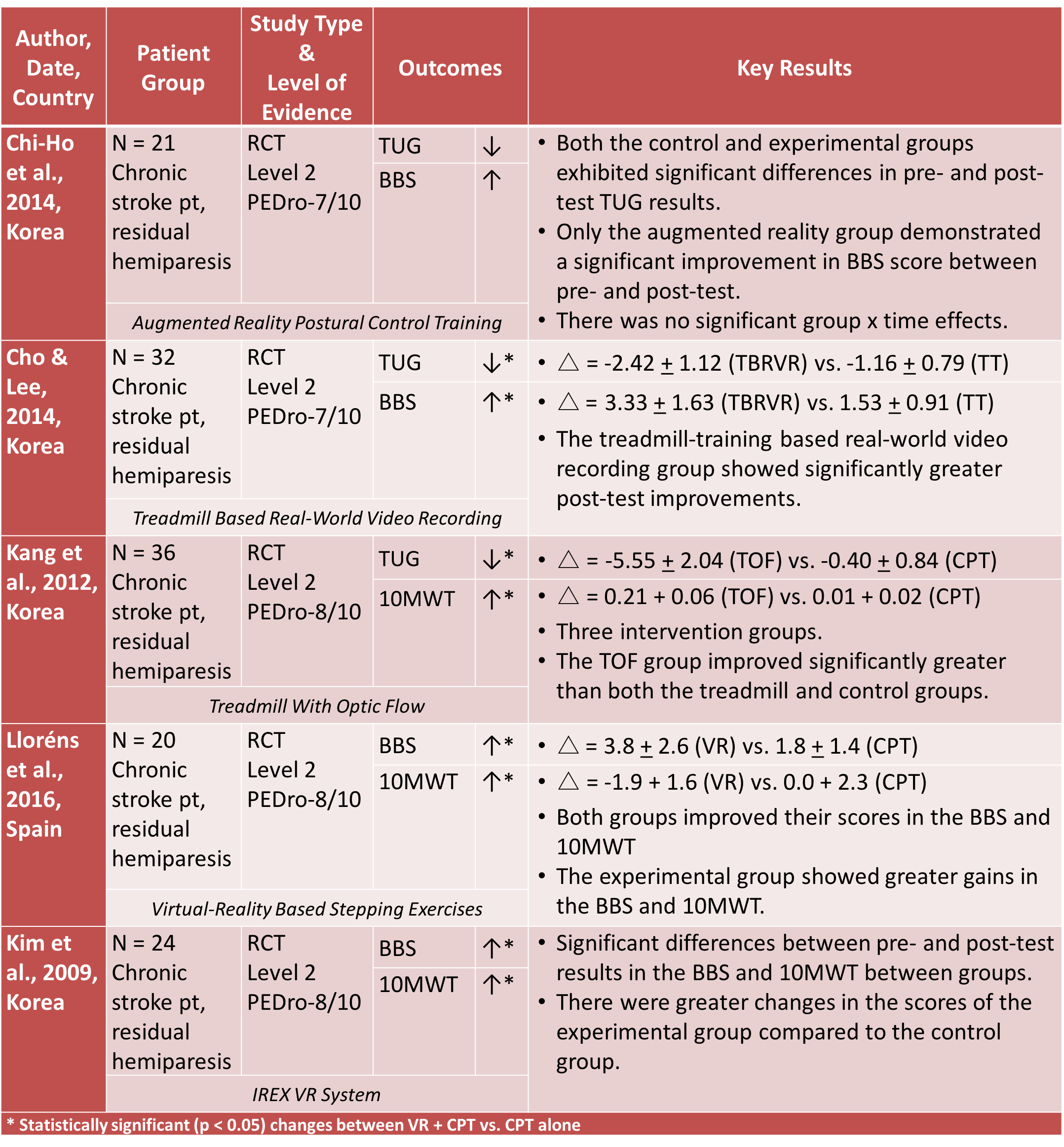
- 3 of 5 articles reported on TUG performance; 2 of 3 studies exhibited moderate-level evidence that VR + CPT leads to significantly greater changes in TUG performance.
- 4 out of 5 articles reported on BBS performance; 3 of 4 articles offer moderate-quality evidence that the use of VR + CPT results in significantly better performance on the BBS.
- 3 out of 5 articles examined 10MWT performance; all 3 articles offer moderate-quality evidence that VR + CPT leads to statistically significant ↑ in gait speed.
Overall, 4 of 5 studies show that VR when combined with CPT has additive effects and improves balance and gait outcome measures when compared to CPT alone.
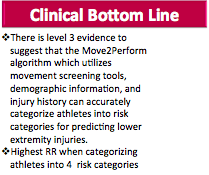
Clinical Bottom Line:
There is limited, moderate-level evidence that suggests that virtual reality in addition to physical therapy is more effective than physical therapy alone in improving gait and balance outcome measures.
Limitations of the Evidence:
- Small sample sizes were utilized in all of the studies.
- There was an inconsistence across the studies of the blinding of therapists, raters, and participants.
- All samples utilized a sample of convenience, limiting the ability to generalize these results to the general stroke population.
- All studies utilized strict inclusion and exclusion criteria limiting the generalizability to the general stroke population.
- All studies only included participants that were ambulatory with high cognitive abilities which does not depict all stroke survivor abilities.
- There was an inconsistence in control group demographics across all 5 studies.
- Not all studies utilized the same methods to implement standard physical therapy or virtual reality limiting our ability as providers to determine the best way to implement virtual reality in addition to normal physical therapy in a plan of care.
- All studies were completed outside of the United States.
- There is an inconsistence across available literature about what the definition of virtual reality is.
- A lot of studies had to be eliminated from this critically appraised topic due to their use of video gaming systems as methods to implement virtual reality within their study.
Recommendations for Future Research:
Overall, there are many opportunities for future research to improve research on virtual reality in chronic stroke patients. In future research, there should be a clearer definition in what constitutes virtual reality. Currently, there is such an inconsistent interpretation of what constitutes virtual reality and the implementation of virtual reality. Many current studies utilize video game consoles and televisions as virtual reality treatment; however, all studies that utilized video games consoles were excluded from this CAT, significantly limiting the available research. Future research should also standardize what constitutes conventional physical therapy treatment, as it is difficult to implement and generalize vastly different conventional physical therapy programs into one physical therapy program. In addition, in future research, larger sample studies should be utilized to increase the statistical power and significance of future research, leading to the ability to generalize this research to the general chronic stroke population. Future research should also implement long-term follow-up periods to determine the long-term retention effects of the additive effects of virtual reality treatment.
Conclusion and Application to Case Scenario:
This evidence supports the notion that virtual reality in additional to conventional physical therapy will significantly improve these balance and gait outcome measures. Based on the current literature, integrating the use of virtual reality into a conventional physical therapy treatment program proves to be more superior than utilizing standard physical therapy alone for balance and gait deficits in chronic stroke patients with residual hemiparesis. Overall, throughout this literature, there have been no adverse events associated with the use of virtual reality; based on this information, the benefits by far outweigh the potential harm. Although there are proven benefits of implementing virtual reality in conjunction to a conventional physical therapy program, it is expensive to invest in virtual reality technology; therefore, its utility may vary depending on patient volume, finances in any given clinic environment, and space in any given setting. By showing that there are no negative consequences to utilizing virtual reality in addition to conventional physical therapy for chronic stroke patients with residual hemiparesis, may prompt more clinics to integrate virtual reality in their treatment program.
In this scenario, Mrs. Cooke presents to an outpatient clinic with balance and gait deficits following a stroke that resulted in residual hemiparesis. This condition and these deficits fall within the scope of current virtual reality research and within a physical therapist’s scope of practice. Since this is the case, the physical therapist may elect to include virtual reality into Mrs. Cooke’s conventional physical treatment program. By integrating virtual reality into Mrs. Cooke’s treatment program, she will have the opportunity to interact with an environment that is similar to the real-world while in a controlled and safe situation. In addition, by including virtual reality in addition to a conventional physical therapy program, Anita will have the ability to receive real time feedback to provide further improvements in her balance and gait outcome measures.
Although most of these research studies have proven the effectiveness of the use of virtual reality in addition to an individualized conventional physical therapy treatment program, there are several gaps in the evidence that lead to difficult application to this clinical question and scenario. The largest gap in the application to this case scenario is that within research that there was no common method of implementing virtual reality therapy or in the standardization of conventional physical therapy throughout these studies. In addition, all of these research studies were performed outside of the United States. Lastly, although the intervention and comparison groups were fairly similar across all studies, there was a large diversity in population as they were not standardized throughout the research.
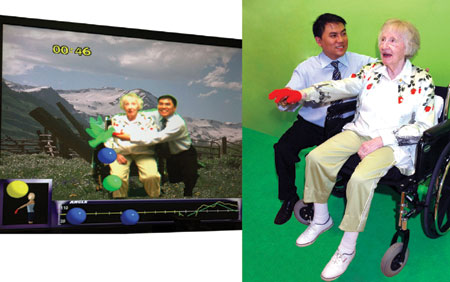
After reviewing the literature, it will be beneficial to integrate the use of virtual reality technology into a conventional physical therapy treatment program for Mrs. Cooke. Anita’s treatment program should include both an individualized conventional therapy treatment program that is based on both the neurodevelopmental and motor learning theory. Anita should participate in physical therapy four times per week, for a total of 70-minute sessions with 40-minutes being dedicated to conventional physical therapy and 30-minutes of virtual reality treatment with the IREX VR system.
Obtained from: http://www.gesturetek.com/images/press/media-oct29-09-3.jpg
Virtual Reality Training should utilize various games on the IREX VR system in order to encourage active lower-limb movement, weight shifting, and single-limb stance. This will facilitate improvement in balance, mobility, stepping and ambulation skills, while simultaneously increasing her strength and range of motion.The difficulty of the games should be increased as Mrs. Cooke makes improvements in order to maximize her ability to progress. Weight and therabands can be added to provide external resistance and make the games harder and promote increased muscle strength and endurance.
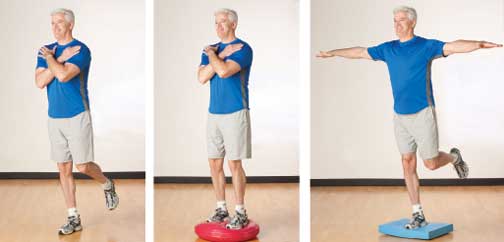
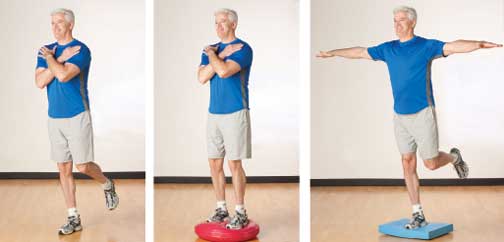
Obtained from: https://acewebcontent.azureedge.net/certifiednews/BalanceExer2.jpg
The conventional physical therapy should be designed to be patient-specific and progress from static balance training to dynamic balance training. Since Anita is independent in quiet static standing balance, Anita would benefit most from progressing from static balance activities within the first few sessions as soon as she is able to shift her weight in the anteroposterior and mediolateral planes while performing functional reaching tasks. Her PT program should also include strengthening for the gluteus medius to improve controlled mobility of the pelvis during the stance phase of gait because she is having difficulty walking, particularly on uneven ground. Anita’s program should also include gait training and dynamic balance on unstable surfaces, because one of her main goals is to be able to walk around her neighborhood again.
References:
- Stroke facts. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/stroke/facts.htm. Updated 20152016.
- National Stroke Association Web site. http://www.stroke.org/we-can-help/survivors/stroke-recovery/post-stroke-conditions/physical/hemiparesis. Accessed October 16, 2016.
- Cho K, Lee W. Effect of treadmill training based real-world video recording on balance and gait in chronic stroke patients: a randomized controlled trial. Gait & Posture [serial online]. 2014;39(1):523-528. Available from: MEDLINE, Ipswich, MA. Accessed September 11, 2016.
- Chi-Ho L, Yumi K, Byoung-Hee L. Augmented reality-based postural control training improves gait function in patients with stroke: Randomized controlled trial. Hong Kong Physiotherapy Journal [serial online]. December 2014;32(2):51-57. Available from: CINAHL, Ipswich, MA. Accessed September 11, 2016.
- Kang H, Kim Y, Chung Y, Hwang S. Effects of treadmill training with optic flow on balance and gait in individuals following stroke: randomized controlled trials. Clinical Rehabilitation [serial online]. March 2012;26(3):246-255. Available from: CINAHL, Ipswich, MA. Accessed September 11, 2016.
- Lloréns R, Gil-Gómez J, Alcañiz M, Colomer C, Noé E. Improvement in balance using a virtual reality-based stepping exercise: a randomized controlled trial involving individuals with chronic stroke. Clinical Rehabilitation [serial online]. March 2015;29(3):261-268. Available from: Psychology and Behavioral Sciences Collection, Ipswich, MA. Accessed September 11, 2016.
- Kim J, Jang S, Kim C, Jung J, You J. Use of virtual reality to enhance balance and ambulation in chronic stroke: a double-blind, randomized controlled study. American Journal Of Physical Medicine & Rehabilitation / Association Of Academic Physiatrists [serial online]. September 2009;88(9):693-701. Available from: MEDLINE, Ipswich, MA. Accessed September 11, 2016.
Please contact Cara Fowler at cara.fowler@temple.edu with any additional questions you may have regarding this topic.