Background:
It is well documented that survivors of stroke are at an increased risk of falls relative to age-matched controls.1,2 Ability to take a reactive step is paramount in recovery from an unexpected loss of balance.3,4 Therefore impaired reactive stepping has been proposed as one important component of the multivariate nature of falls following a stroke. One value that has been the topic of discussion in reactive stepping literature is the TFO, or time to foot off. This measure represents the time between the release of external support of an individual leaning their center of mass (anteriorly) outside of their base of support, to the time in which their body weight is no longer supported by the limb in which they choose to step. Characteristics of impaired reactive stepping have been shown to correlate with falls in elderly populations.2

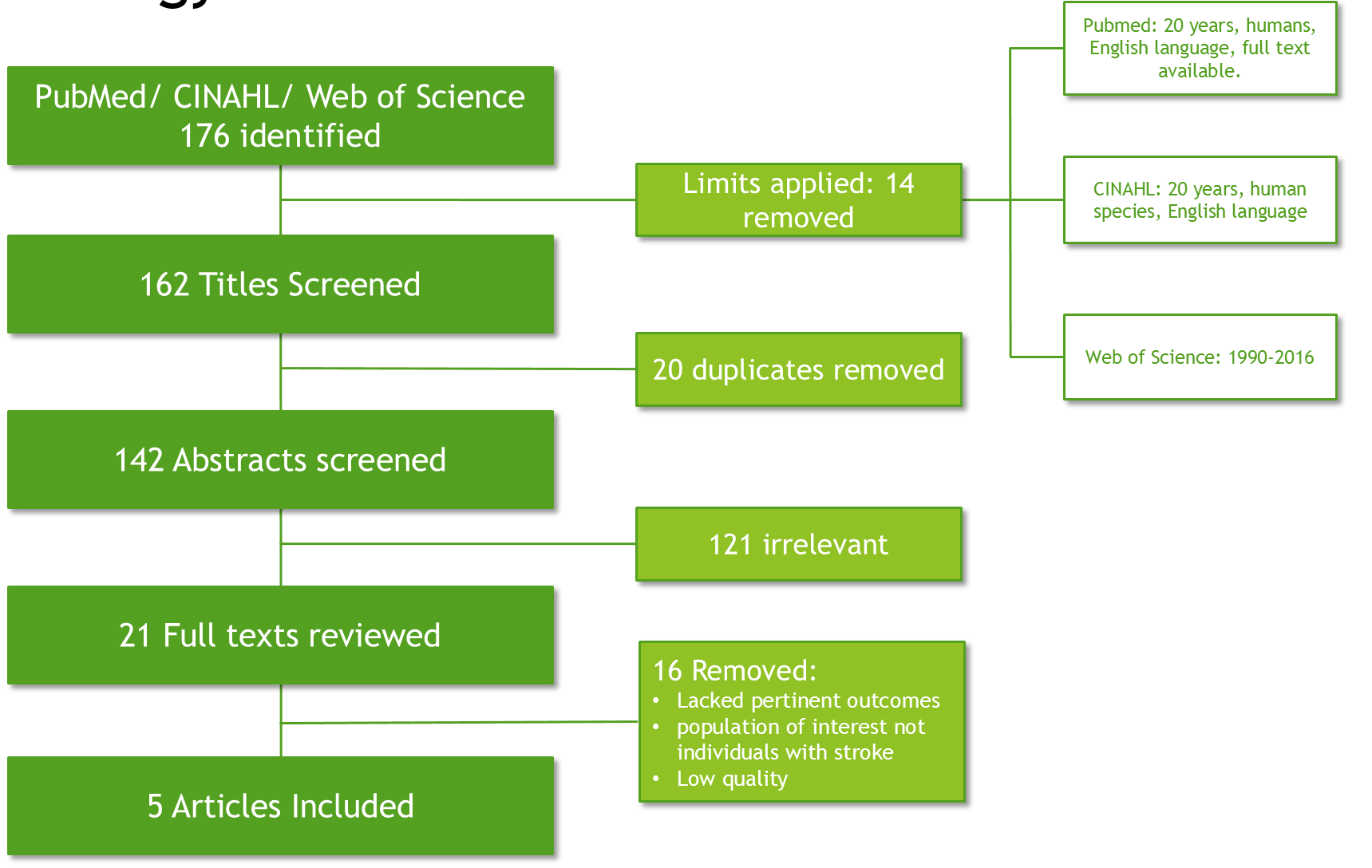
Search Strategy:
Pub Med: Search Terms: (((stepping) OR reactive stepping) AND poststroke) OR reactive stepping[Title/Abstract]
CINAHL: Boolean/phrase: reactive stepping OR stepping AND poststroke
WOS: Search strategy : TITLE: (reactive stepping) AND TOPIC: (stroke)
Inclusion Criteria:
-Participants must be above the age of eighteen and had their neurologic incident at least two weeks prior to enlisting in the study in order to be considered ‘chronic.’
-The methodology of how the researchers obtained values related to perturbation or reactive response must be clearly explained within the article.
-At least one outcome related to falls in the stoke population must have been collected.
Exclusion Criteria
-Articles which only examined metrics on gait or focused on outcomes related to gait.
-Level V evidence
Rationale for data collection:
A lack of association between reactive stepping impairment and utilized clinical measures (BBS, gait velocity, STRATIFY falls risk tool) has been identified. This suggests a limitation may exist when drawing inferences with these measures to predict likelihood of falls. Therefore we may be missing a critical evaluative component in this patient population, which could also help us streamline our intervention. In addition, falls render increased healthcare utilization and diminished quality of life of affected individuals.
Methods:
-Setting and participants:
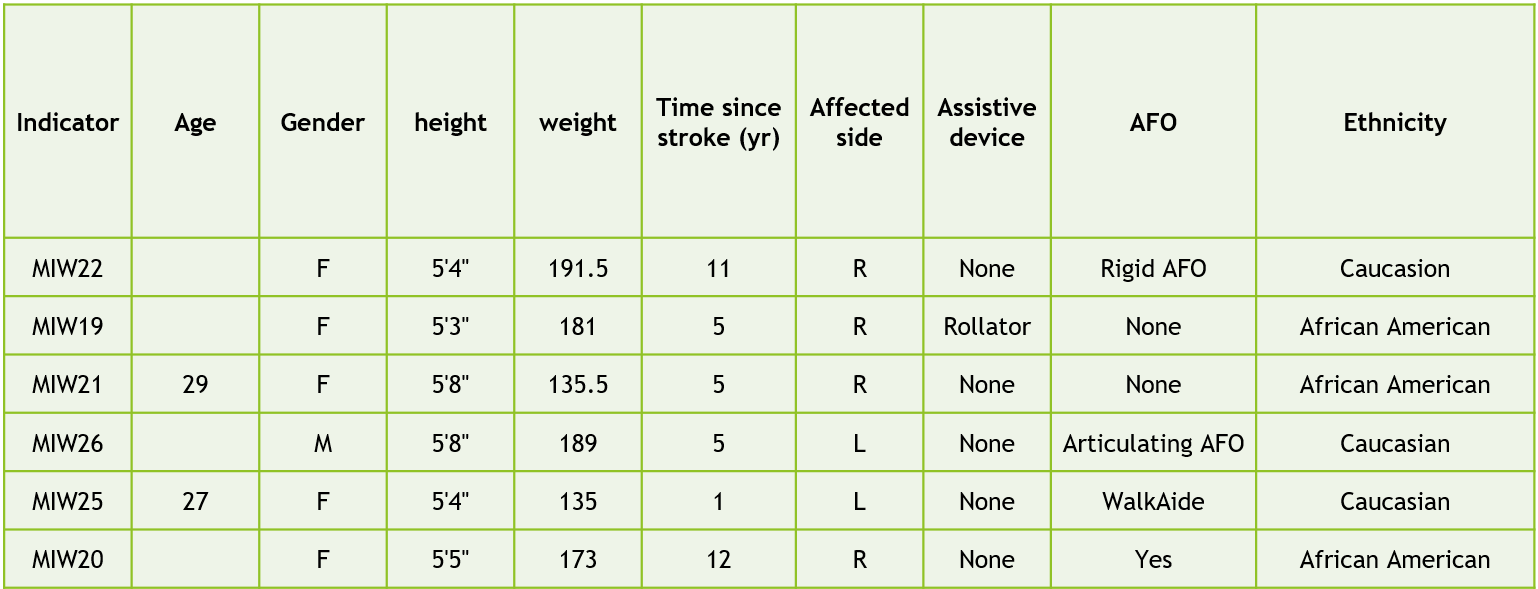
Leahy lab at the University of the Sciences in Philadelphia. Subjects (n=6) recruited as part of a larger study at the university lab investigating moderate intensity walking in people with stroke. Subjects recruited from local physical therapy clinics, stroke support groups, and individuals who have participated in research and classroom activities previously at the USciences Department of Physical Therapy. Healthy controls (n=5) are healthcare students recruited by convenience.
Inclusion:
-People over the age of 18 years with one or more strokes at least 3 months previously
-Ambulatory without physical assistance of other person (orthotic devices, canes or walkers will be allowed)
-Able to follow instructions and able to communicate with investigators as assessed by specific NIH Stroke Scale questions.
Exclusion:
-Bone or joint problems that limit the ability to walk
-Resting hear rate outside of the range of 40-100 beats per minute
-Resting blood pressure outside of the range of 90/60 to 170/90 mm Hg
-Chest pain or shortness of breath with exertion
-Score of >1 on question 1b and >0 on question 1c on the NIH Stroke Scale inability to communicate with investigators.
Demographics:
Control group:

Affected group:
Upon entering clinic individuals were oriented to the purposed of the study, screened to be deemed fit for inclusion, and consented for participation. Then the following outcomes were collected: TUG, TUGmanual, TUGcognitive, 6MWT, 4 square step test (modified if unable), gait velocity-preferred, and gait velocity-fast.
They then underwent the reactive stepping assessment. They underwent five trials where they were able to step with whatever limb they desired. Following this five trials were done while blocking the preferred limb in an attempt to elicit a step with the non-preferred limb.
The method for each trial is as follows:
- Participant is to stand statically in their preferred foot position inside of a body weight support system designed to catch them if an attempt to regain balance is failed.
- Patient will be positioned on a GaitRite system. (Collecting data through ProtoKinetics Movement analysis software)
- A gait belt is then locked into a closed loop around the patient by tester #1 and placed outside of the subject’s shoulders, utilizing the acromion bilaterally as the landmark of standardization.
- A Lafayette Manual Muscle Testing myometer is then placed inside of the gait belt (with the screen visible to tester #1) so as to garner the force paced upon it when the gait belt pulls forward, as described in step #6.
- Tester #1 checks to make sure both feet are in alignment before having subject lean.
- As tester #1 holds the myometer statically in place, the individual is instructed to progressively lean forward into the gait belt until 8-10% of their precalculated bodyweight is displayed on the readout. The subject is then instructed to hold this position as best they can.
- The subject is then released 2-10 seconds after they are instructed to hold their ‘forward leaning’ position with the desired % body weight. At this time the subject is release by tester #1, inducing a reactive stepping response. If at any point the subject falls outside of the 8-10% range of their bodyweight, the process will be started over again from step #4.
Data Extraction
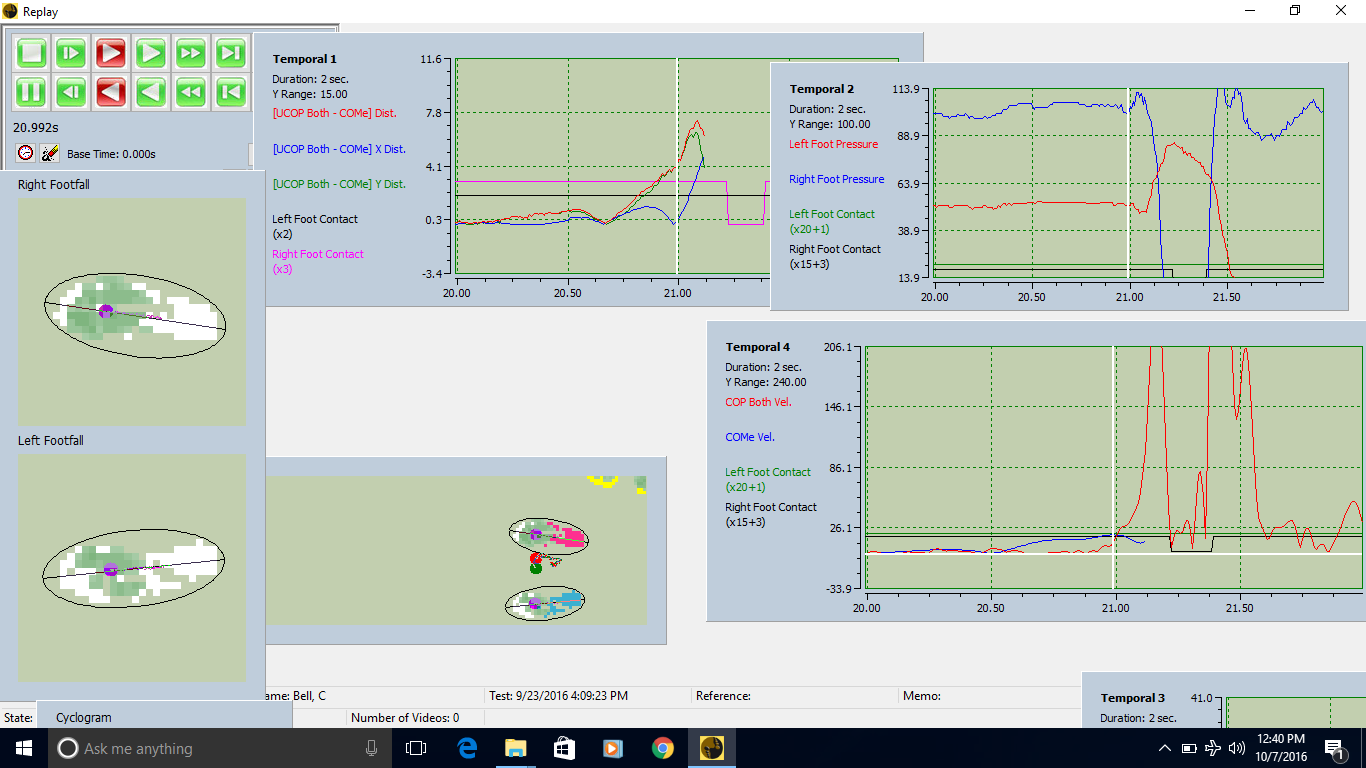
Extracting the TFO value was done utilizing the PKMAS software system for the GaitRite mat. In the photo below the box labeled ‘temporal 4’ gives the indication of when the subject was released through the sharp increase in slope of the center of pressure (red) reading. This time is noted, and the time at which pressure is no longer picked up by the stepping limb is noted. The time between these two values is noted. The GaitRite mat has a sampling rate of 120 Hertz, therefore frames are captured every 8 milliseconds.
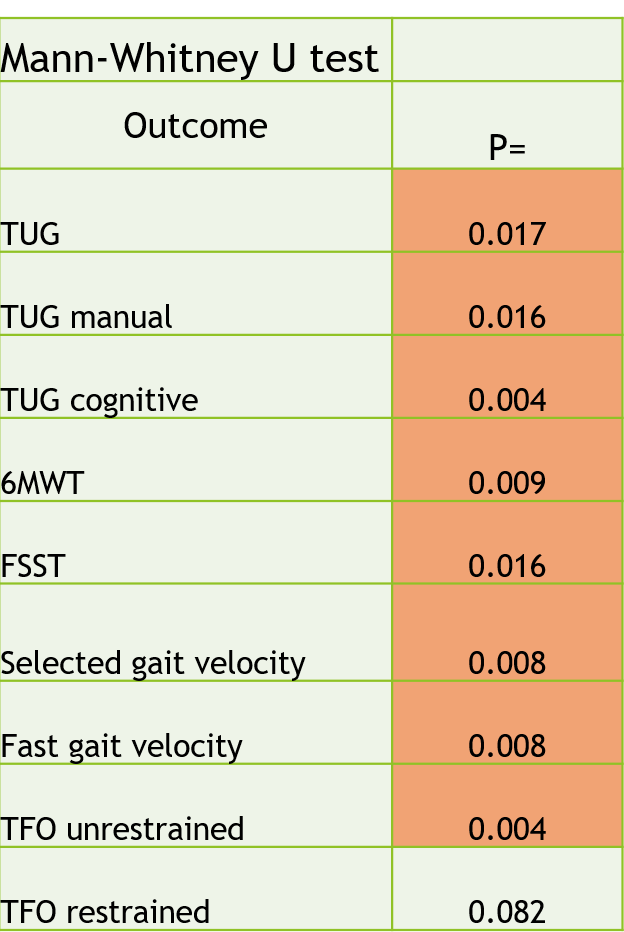
Statistical analysis:
Nonparametric
Independent-samples Mann-Whitney U test
-To identify between-group differences in TFO and outcome measures
Spearman rank correlation coefficient (Spearman’s rho)
-To identify correlation between TFO and outcome measures
Wilcoxon signed-ranks test
-To identify between-limb differences in stroke and control group
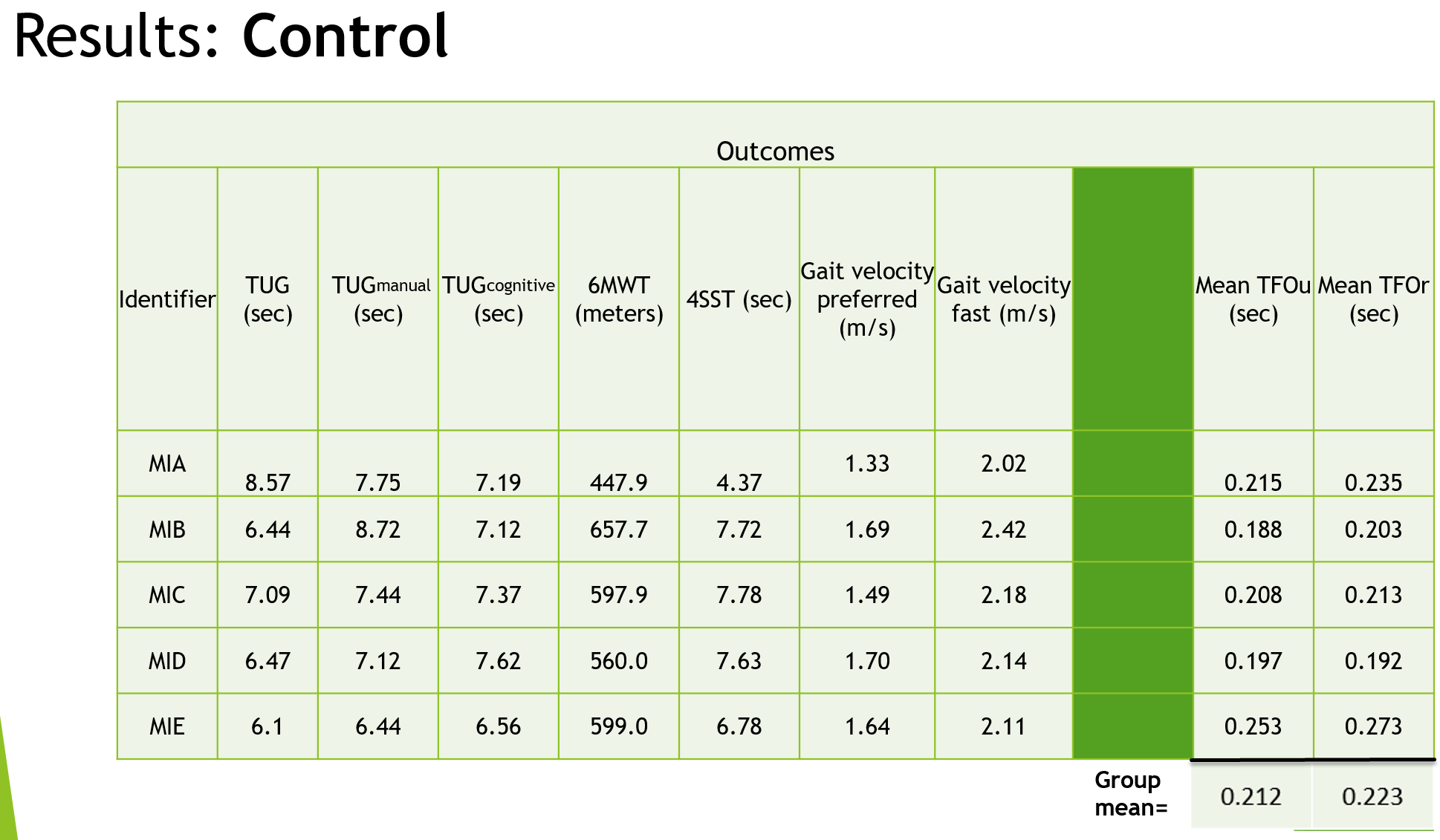
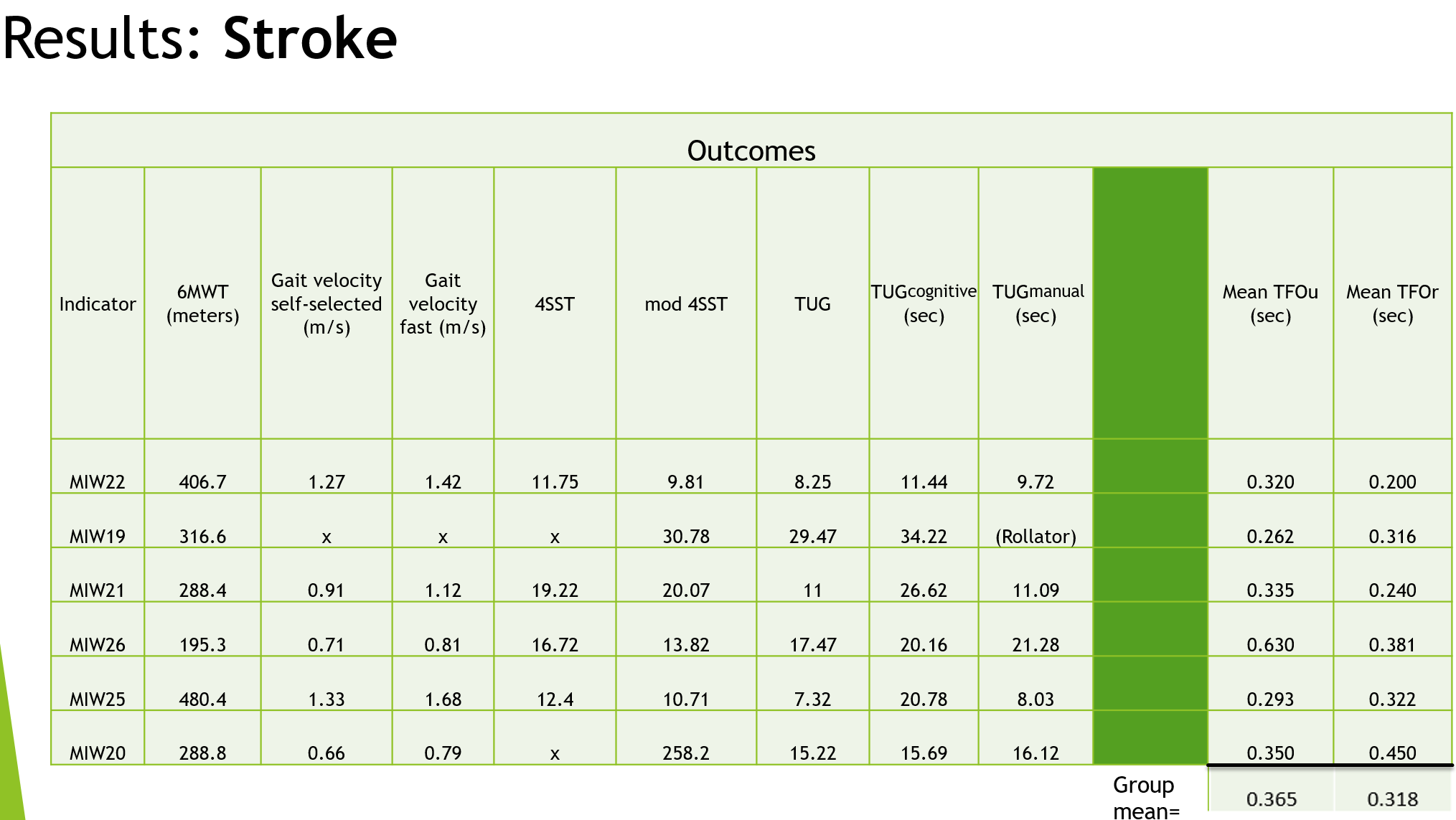
Results:
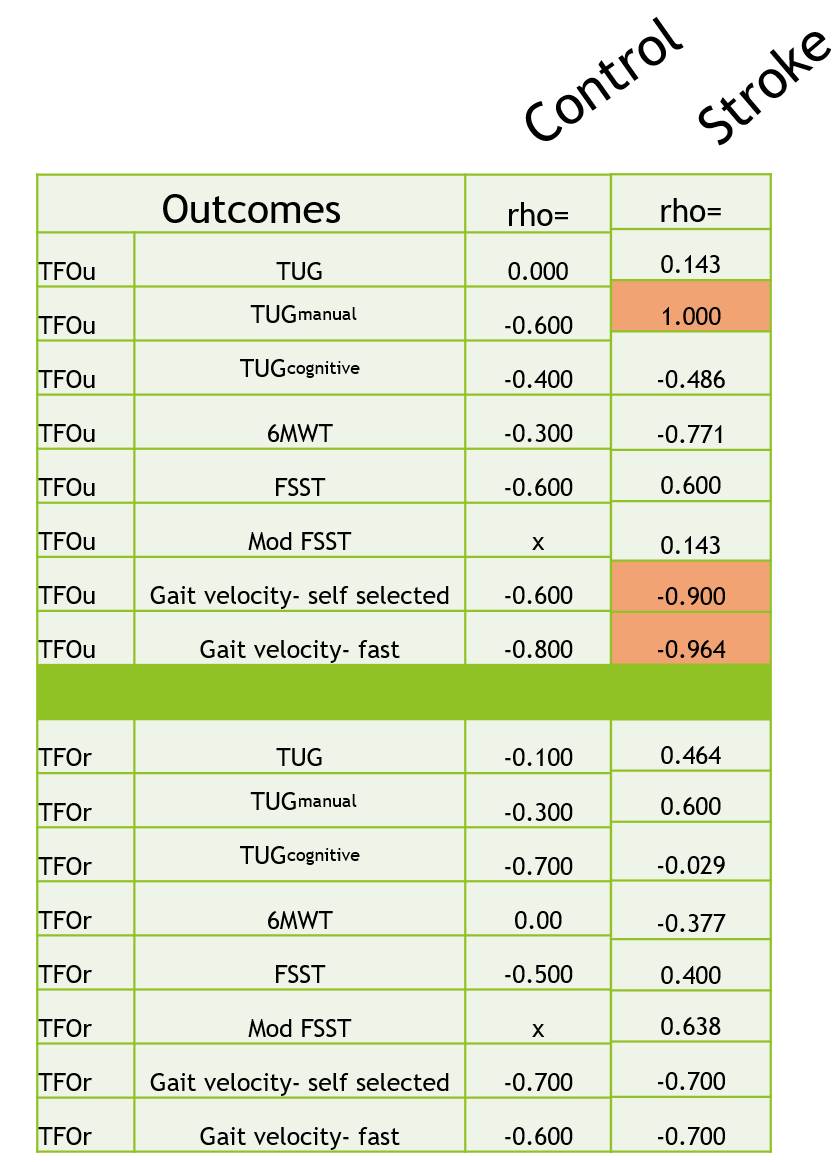
**Red indicates statistical significance
Wilcoxon Signed ranks test
-No significant difference between TFOu and TFOr in either group.
M-WU:
Limitations:
-Inherent limitation in methodology (e.g. handheld myometer use). Non age-matched controls from sample of convenience. Small sample size limits generalizability and ability to establish validity.
Suggestions for future research:
Larger sample sizes. Research individuals who have experienced a stroke compared to age-matched cohort. Correlate TFO values with fall rates in the community. Explore utility of this measure as an outcome and how it responds to interventions. Cost-effective methods of collecting value in outpatient realm.
Citations
1.Maki B, Edmonstone M, Perry S, Heung E, Quant S, McIlroy W. Control of rapid limb movements for balance recovery: do age-related changes predict falls risk? Control of Posture and Gait. Maastricht, the Netherlands: International Society for Postural and Gait Research; 2001: 126-129.
2.Hilliard MJ, Martinez KM, Janssen I, et al. Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil. 2008;89: 1708-1713
3.Maki BE, McIlroy WE. The role of limb movement in maintaining upright stance: the “change-in-support” strategy. Phys Ther. 1997;77: 488-507.
4.Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age Ageing. 2006;35(suppl 2): ii12-ii18.
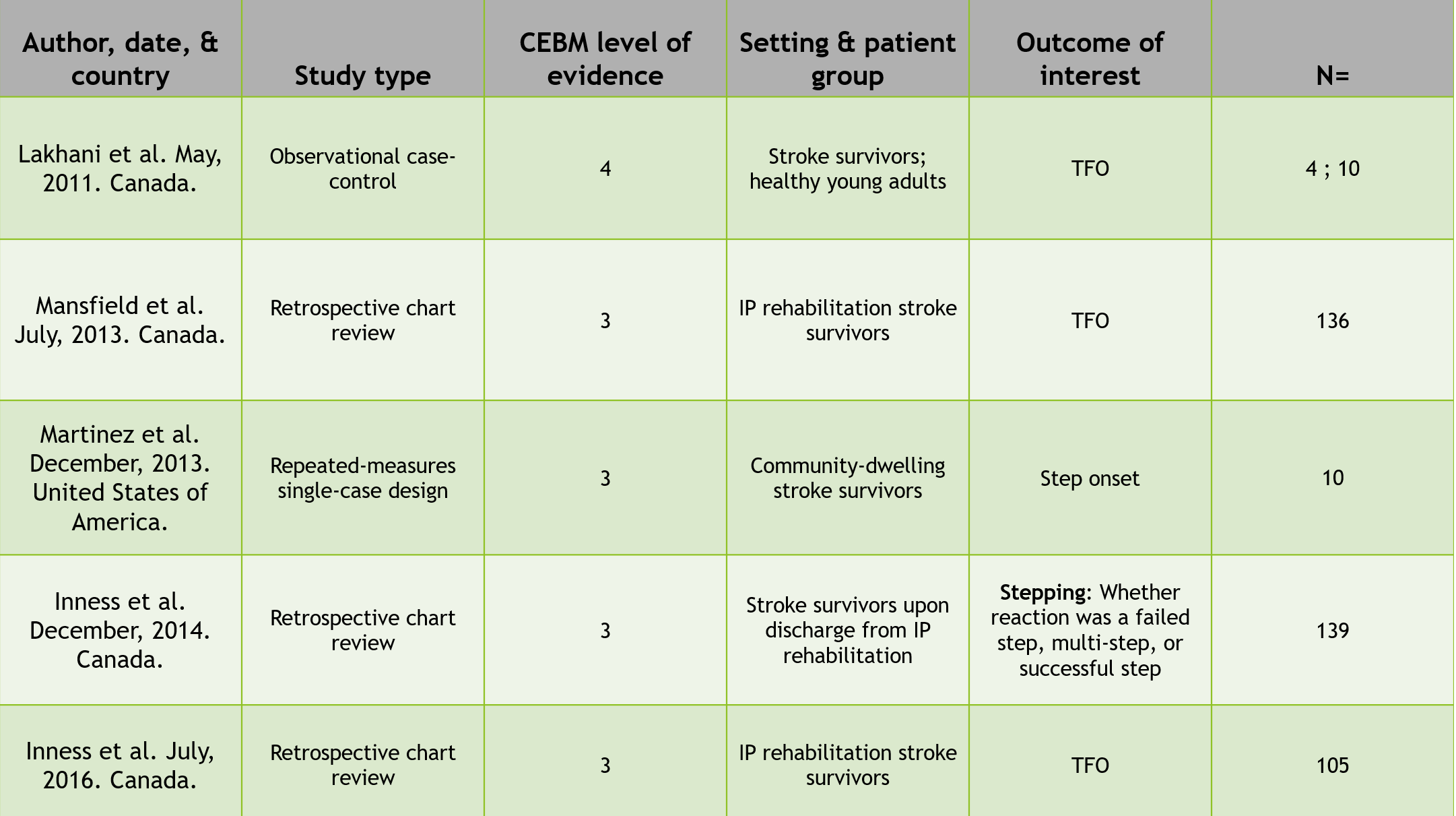
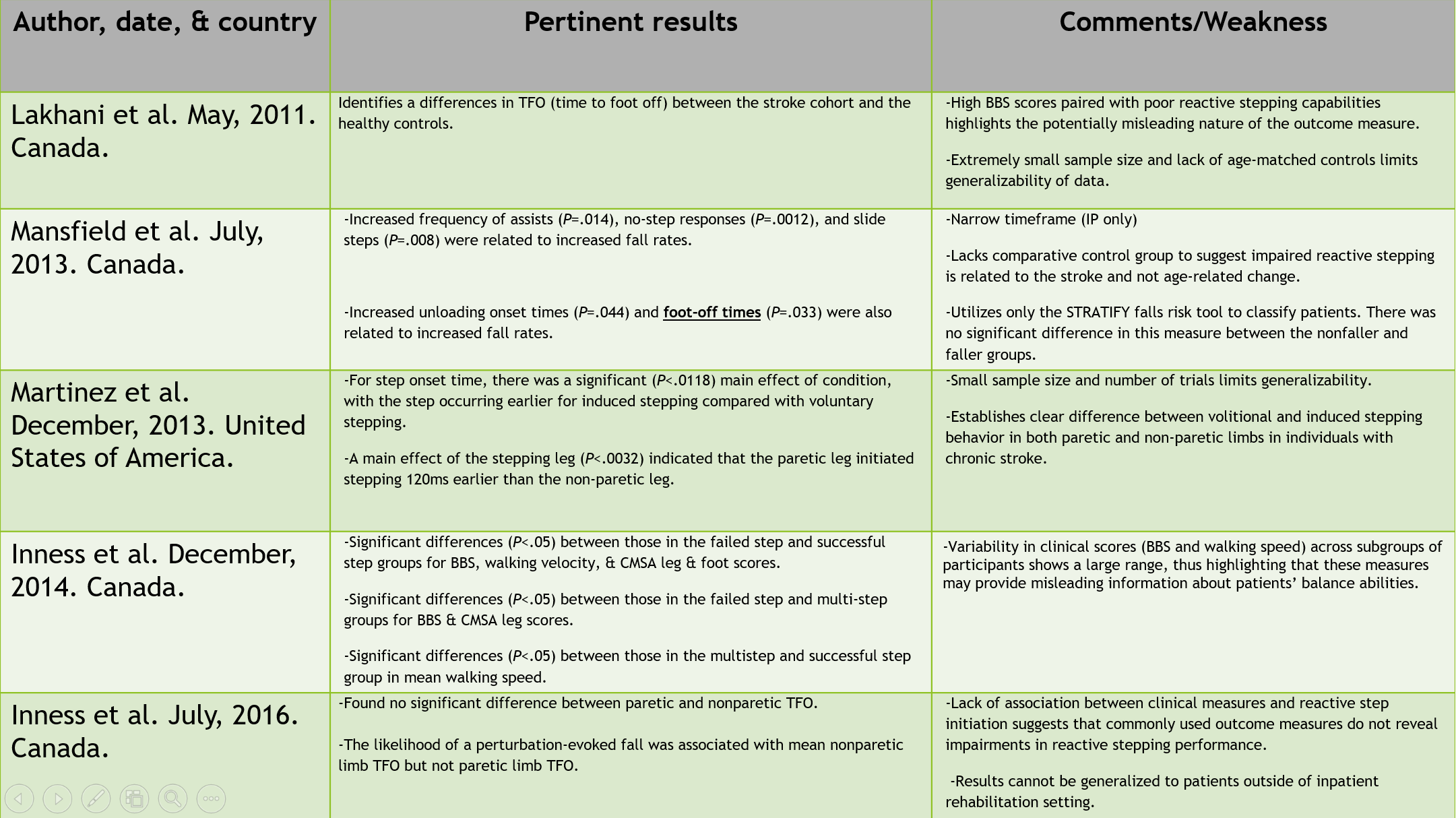
5 articles from search:
- Mansfield A, Inness EL, Wong JS, Fraser JE, McIlroy WE. Is impaired control of reactive stepping related to falls during inpatient stroke rehabilitation? Neurorehabil Neural Repair. 2013;27:526-33.
- Inness EL, Mansfield A, Lakhani B, Bayley M, McIlroy W. Impaired reactive stepping among patients ready for discharge from inpatient stroke rehabilitation. Phys Ther. 2014;94:1755-64.
- Martinez KM, Mille M, Zhang Y, Rogers MW. Stepping in persons poststroke: comparison of voluntary and pertubation-induced responses. Arch Phys Med Rehabil. 2013; 94:2425-32.
- Inness EL, Mansfield A, Bayley M, McIlroy WE. Reactive stepping after stroke: determinants of time to foot off in the paretic and nonparetic limb. Journal of Neurologic Physical Therapy. 2016; 40:196-202.
- Lakhani B, Mansfield A, Inness E, McIlroy WE. Compensatory stepping responses in individuals with stroke: a pilot study. Physiotherapy Theory and Practice. 2011; 27(4): 299-309.