Background:
Preterm birth is the birth of an infant before 37 weeks of pregnancy. In 2014, preterm birth affected about 1 of every 10 infants born in the United States. Preterm birth is the greatest contributor to infant death. Most preterm-related deaths occurring among babies who were born very preterm (before 32 weeks). Preterm birth is the leading cause of long-term neurological disabilities in children. Some problems that premature infants may face include: breathing problems, feeding difficulties, cerebral palsy, developmental delay, vision problems and hearing impairment.1
 4
4
Case Scenario:
My patient is currently a 32 weeks gestational age female who was born at 26 weeks gestational age. From the time of birth, the patient has been in the NICU of the local hospital. Upon evaluation, the patient has present grasp reflexes bilaterally (UE and LE), absent Babinski bilaterally, present rooting reflex bilaterally, one beat of clonus on the right lower extremity and two beats of clonus on the left lower extremity. The patient has increased tone in all extremities, a 1 on the modified Ashworth scale in all extremities. The patient has normal range of motion in all extremities and neck. The patient prefers right neck rotation while in supine but can tolerate left neck rotation if put in that position. The patient had mostly stable vital signs throughout the treatment, with two O2 sat drops into the low 80s which the patient was able to independently recover from when treatment was paused. Throughout the examination and treatment, the patient had minimal fussing.
PICO Question:
In premature infants, what effect does physical therapy in the first 6 months of life have on motor development?
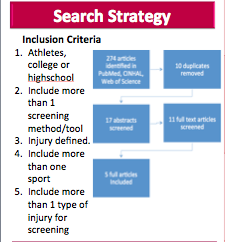
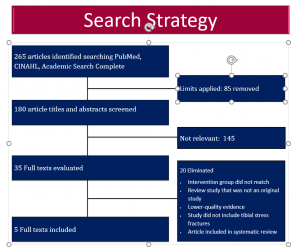
Search Strategy:
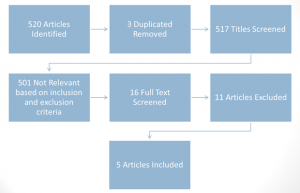
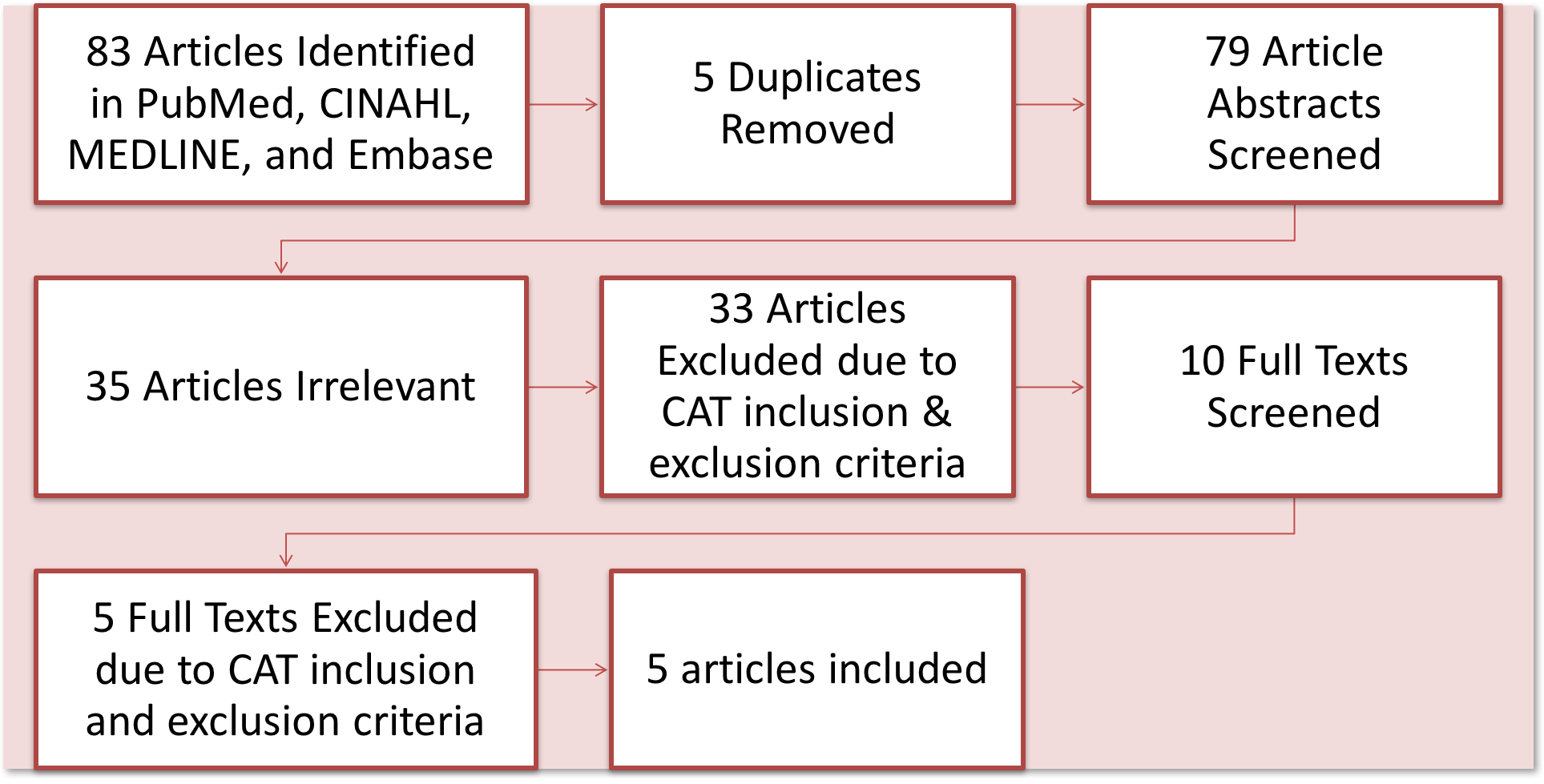
Three databases were searched: Pubmed, Cinahl and Ovid. The key words “premature infants”, “physical therapy”, “neonatal intensive care unit” were used to search. The limits English language and article published from the year 2000 to the present were applied and and resulted in a total of 520 articles. 3 Duplicate articles were removed. 517 Titles were screened. Articles were excluded if they did not relate to physical therapy, motor development or intervention within the first 6 months of life in premature infants. 501 articles were not relevant, leaving 16 articles for full text screening. 11 of those articles were excluding leaving 5 articles to include.
Article 1- Lekskulchai et al, 2001:
CEBM Level 2 of Evidence; RTC; PEDro = 7/10
The population in this study included 111 premature infants gestational age < 37 weeks (Thailand). The interventions were individualized to the patient but included: positioning techniques, assisted kicking, promotion of eye following head movement, encouragement of weight bearing, assisted rolling, promoting reaching, encouragement of head righting. In this study and all of the studies that were looked at, the physical therapist trained the primary care giver who performed the interventions with the infants. The results of this study were that the intervention group showed significantly better results on the Test of Infant Motor Performance than the control group after 4 months.
Clinical bottom line: A developmental physical therapy program was found to be useful in promoting motor performance of preterm infants who were detected as being at risk for developmental delays during the early stage of life. 3
Article 2-Heathcock et al, 2009:
CEBM Level 2 of Evidence; RTC; PEDro = 5/10
The population in this study included 27 preterm infants gestational age < 33 weeks and weight < 2,500 g (United States). For the intervention group, there was 3 categories of interventions: General movement of lower extremity (ex: attaching bells onto the infant’s sock and encouraging foot-toy interaction), Midline movement (ex: holding a toy in midline reach and encouraging infant to make contact to the toy with their foot), Distinct movement (ex: caregiver holds infant’s hip at 90 degrees and encouraging primarily knee motion to contact the toy). The results of this study were that the intervention group had significantly more average number of foot-toy contact, mean foot-toy duration and percentage of infants that touched the toy more than 10 times at 8 weeks.
Clinical bottom line: Physical therapists can use feet-oriented play as an intervention technique with premature infants in the first 6 months of life to increase the rate of motor development. 2
 2
2
Article 3- Heathcock et al, 2008:
CEBM Level 2 of Evidence; RTC; PEDro = 6/10
The population in this study included 26 preterm infants gestational age <33 weeks and weighted < 2,500g (United States). The intervention group received 3 categories of activities: General movement( ex: holding a toy attached to the infant’s sleeve so that any arm movement causes movement of the toy), Midline movement(ex: encouraging the infant to touch a toy held at midline), Distinct movement (ex: caregiver holds the infant’s upper arm and holds a toy over the infant’s hand, encouraging elbow movement). The results of this study were that the intervention group had significantly more hand-toy contacts, longer hand-toy duration and number of infants that contacted the toy more than 5 times at 8 weeks.
Clinical bottom line: Physical therapists can use arm reaching activities as an intervention technique in premature infants in the first 6 months of life to help improve gross motor skills. 4
 4
4
Article 4- Cameron et al, 2005:
CEBM Level 2 of Evidence; RTC; PEDro = 6/10
The population in this study included 72 Preterm infants gestational age >24 weeks (United Kingdom). After the start of the study, Twelve (20%) of the preterm sample were diagnosed with cerebral palsy, most of these infants from the treatment group. The effects of these infants may have balanced out the median Alberta Infant Motor Scale scores in the results. The treatment group received individualized interventions including handling and positioning techniques, designed to promote symmetry and muscle balance and movement using postural support and facilitation techniques. The results of this study were that there was no difference in the Alberta Infant Motor Scale between the intervention and control group at 4 months. However, this study also found that in the intervention group, infants with good parental compliance scored significantly better on the Alberta Infant Motor Scale than moderate or poor parental compliance.
Clinical bottom line: Physical therapy intervention increases motor performance, but not significantly, of infants born very preterm with very low birth weight at four months corrected age. Parental compliance to the intervention program significantly affected motor performance of the infants at four months corrected age. 5
Article 5- Koldewijn et al, 2009:
CEBM Level 2 of Evidence; RTC; PEDro = 6/10
The population in this study included 176 preterm infants gestational age <32 weeks and birth weight < 1,500g (Netherlands). This study used the Infant Behavioral Assessment and Intervention Program. The motor development strategies used in this program focus on midline orientation (ie. brining hands together and hands to mouth) and are also used to enhance postural control (ie. head and body righting in different positions) with the aim of addressing specific motor problems in preterm infants. The results of this study were that the intervention group had significantly better results on the Behavioral Rating Scale but not on the Infant Behavioral Scale at 6 months.
Clinical bottom line: The Infant Behavioral Assessment and Intervention Program improved outcomes, though not significantly, of premature infants at 6 months corrected age. 6
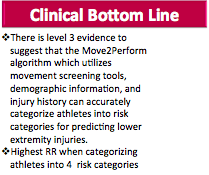
Clinical Bottom Line:
There is moderately high level research that shows physical therapy in premature infants in the first 6 months of life can increase motor development in the short term
 4
4
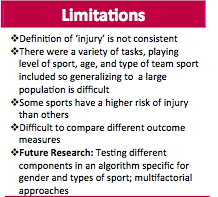
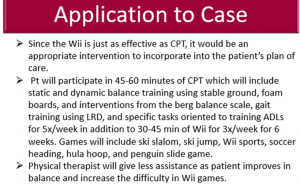
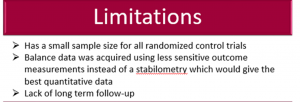
Limitations:
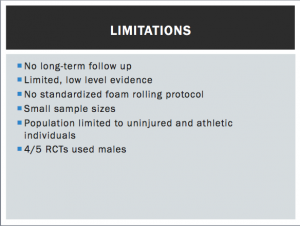
The premature infants in all of these randomized controlled studies that have been shown to benefit from physical therapy are relatively healthy and do not have congenital abnormalities, genetic disorders, prenatal drug exposure, vision and hearing problems. Therefore, no effects of physical therapy are known for premature infants that may have some of these impairments listed. All of these randomized controlled trials only study motor development effects in the short term and no long term effects have currently been studied. None of the studies blinded the subjects or the physical therapist because it is not ethical. The therapists need to know the intervention in order to coordinate treatment between all of the infant’s health care providers to ensure the infant is receiving the optimal care. It would also be unethical to blind the subjects and the parents of the infants. Many of the studies have a higher dropout rate or small sample sizes. More research needs to be done to assess the effects of physical therapy in the long term, on premature infants with other health conditions and the cost effectiveness of physical therapy as an early intervention for premature infants.
Application:
My patient would be an appropriate candidate for motor development physical therapy because she was born at 26 weeks gestational age and currently does not have any other health conditions that would affect treatment. I would start treatment now at 32 weeks gestational age since my patient is medically stable. I would treat this patient 5 times a week for about 15 minutes a day, depending on tolerance and behavior. My treatment plan would include extremity movement and postural techniques. Since my patient prefers right neck rotation while in supine, I would encourage left rotation actively and position her in left neck rotation when she is in supine. I would progress this to encouraging left cervical rotation while I have her supported in a sitting position. Since my patient has slight increase in tone in all extremities, I would encourage general movement of all extremities using a toy. I would progress this by using a toy to encourage midline movement of her extremities. I would treat my patient for the remainder of her stay in the NICU. When my patient is discharged from the NICU, I would educate and instruct her caregivers to continue the exercises.
Resources:
1.Preterm Birth. CDC. 2015. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm
2.Heathcock J, Galloway J. Exploring Objects With Feet Advances Movement in Infants Born Preterm: A Randomized Controlled Trial. Phys Ther. 2009;89:1027-1038. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3928666/
3.Lekskulchai R, Cole J. Effect of a Developmental Program on Motor Performance in Infants Born Preterm. Australian Journal of Physiotherapy. 2001; 47: 169-176. http://www.sciencedirect.com/science/article/pii/S0004951414602646
4.Heathcock J, Lobo M, Galloway J. Movement Training Advances the Emergence of Reaching in Infants Born at Less Than 33 Weeks of Gestational Age: A Randomized Clinical Trail. Phys Ther. 2008; 88: 310-322. https://www.ncbi.nlm.nih.gov/pubmed/18096650
5.Cameron E, Maehle V, Reid J. The Effect of an Early Physical Therapy Intervention for Very Preterm, Very Low Birth Weight Infants: A Randomized Controlled Clinical Trail. Pediatric Physical Therapy. 2005; 107-119. https://www.ncbi.nlm.nih.gov/pubmed/16357661
6.Koldewijn K, Wolf M, Wassenaer A, Meijssen D, Sonderen L, Baar A, Beelen A, Nollet F and Kok J. The Infant Behavioral Assessment and Intervention Program for Very Low Birth Weight Infants at 6 Months Corrected Age. J Pediatr 2009; 154:33-38. https://www.researchgate.net/publication/221692335_The_infant_behavioral_assessment_and_intervention_program_in_very_low_birth_weight_infants_Outcome_on_executive_functioning_behaviour_and_cognition_at_preschool_age
Please contact Laura Bishop at tuf66520@temple.edu for any further questions.







 4
4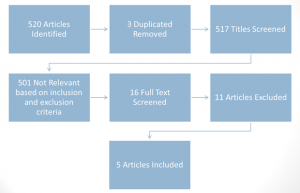
 2
2 4
4 4
4